Статья опубликована на с. 93-97
Введение
Абсцессом головного мозга принято считать гнойную полость, имеющую капсулу [1]. Абсцесс головного мозга может быть результатом распространения инфекции из очага «по-соседству», как при лор-инфекции (оториногенные), переноса инфекции гематогенным путем из первичного очага инфекции, после черепно-мозговой травмы или вследствие хирургических вмешательств. Нередки абсцессы, при которых источник инфекции выявить не удается.
Достижения в микробиологических методах диагностики, антибиотики широкого спектра действия, компьютерная (КТ) и магнитно-резонансная томография (МРТ) привели к значительным успехам в диагностике и лечении абсцессов головного мозга за последние десятилетия. Но, несмотря на все достижения, данное заболевание продолжает оставаться потенциально опасным состоянием для жизни больного и в настоящее время.
Несмотря на успехи в диагностике и лечении, заболеваемость абсцессами головного мозга сохраняется и сегодня на сравнительно стабильном уровне. В США наблюдается около 1500–2000 случаев в год, в развивающихся странах частота существенно выше [2].
Так, в развитых странах заболеваемость абсцессом головного мозга варьирует от 1–2 % от всей внутричерепной патологии, тогда как в развивающихся — до 8 % [7, 20, 26, 30]. Соотношение мужчины/женщины — 1,5–3 : 1 [2].
Широкое использование КТ и МРТ в последнее время значительно улучшило диагностику, хирургическое планирование и исходы лечения пациентов с абсцессами головного мозга [10].
В докомпьютерную эру смертность составляла 22,7–45 % [4, 6, 28], тогда как в настоящее время — 0–20 % [21, 31].
Компьютерная и магнитно-резонансная томография позволяют «увидеть» абсцесс, провести дифференциальную диагностику с метастазами, мультиформными глиальными опухолями высокой степени анаплазии, паразитарными заболеваниями (токсоплазмоз), лучевым некрозом, гематомой в фазе рассасывания [3, 29], а также определить стадию заболевания [8, 9]:
— стадия церебрита: при МРТ-исследовании в Т1-режиме виден очаг пониженной интенсивности, в режиме Т2 — высокий сигнал, при КТ-исследовании видна гиподенсивная зона в белом веществе;
— капсулярная стадия: в режиме Т1 — в центре образования низкий сигнал, по периферии видна капсула с умеренно гиперинтенсивным сигналом, в Т2-режиме — центр гипер- или изоинтенсивный, капсула в виде хорошо очерченного ободка.
При лечении абсцесса головного мозга необходим комплексный подход, включающий как медикаментозную терапию, так и хирургическое лечение.
В зависимости от размера, месторасположения, стадии развития абсцесса используются различные варианты хирургического лечения. Тотальное хирургическое удаление абсцесса, считавшееся до недавнего времени оплотом в нейрохирургии абсцессов головного мозга, стало оспариваться из-за появления стереотаксических методов лечения.
Цель исследования: оценка эффективности различных методов хирургического лечения пациентов с абсцессами головного мозга.
Материалы и методы
Авторами был проведен анализ результатов лечения 242 больных абсцессами головного мозга из 6 областей Украины (Донецкая, Луганская, Киевская, Херсонская, Запорожская, Днепропетровская). Женщин — 78 (32,2 %), мужчин — 164 (67,8 %). Возраст больных — от 1 месяца до 74 лет, средний возраст пациентов составил 36,5 ± 13,8 года.
Все пациенты проходили всесторонние обследования, включавшие анализ анамнестических данных, неврологическое обследование, общеклинические анализы крови, осмотр отоневролога, нейроофтальмолога, производилось КТ- или МРТ-исследование.
Во время оперативного вмешательства у всех больных производили забор содержимого абсцесса для бактериологического посева с целью выделения аэробов, грибов рода Candidа, а также определения чувствительности к антимикробным препаратам.
Результаты и обсуждение
В нашем исследовании абсцесс был одиночным у 190 (78,5 %) больных, многокамерным — у 22 (9,1 %), множественным — у 30 (12,4 %) больных.
У разных авторов частота тех или иных видов абсцессов отличается: одни на первое место ставят контагиозный вид [13, 17, 29], другие — гематогенный [12, 14, 18, 33].
В развитых странах первое место занимают гематогенные абсцессы в связи с успешным лечением синуситов. В нашем исследовании количество гематогенных и контагиозных абсцессов примерно одинаковое — 80 (33 %) и 79 (32 %) соответственно, что свидетельствует о необходимости оптимизации лечения синуситов, своевременного назначения адекватных препаратов для предупреждения тяжелых форм осложнений — абсцессов головного мозга. На рис. 1 приведены наши данные.
В нашем исследовании преобладала тактика хирургического лечения в комбинации с антибактериальной терапией. Из 242 пациентов прооперированы 233 (96,3 %), не оперированы только 9 человек (3,7 %).
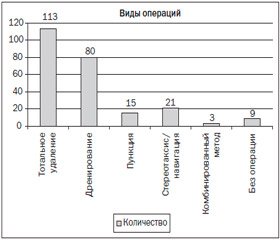
Все хирургические вмешательства, произведенные в нашем исследовании, можно разделить на следующие виды:
1) тотальное удаление абсцессов вместе с капсулой (иногда выполнялось частичное удаление капсулы из-за ее интимного сращения с тканью мозга или ее разрыва);
2) пункция и дренирование абсцесса, использовался как один дренаж, так и система «приток — отток»;
3) пункционный метод без применения навигационных систем, «от руки», без установки дренажей;
4) операции с использованием рамочной или безрамочной навигации, как удаления, так и пункции;
5) комбинированный метод: на первом этапе проводилась пункция или дренирование, на втором — удаление абсцесса с капсулой.
Рассмотрим более детально каждый из методов оперативного лечения.
На первом месте по количеству произведенных операций — тотальное удаление абсцесса. Выполнено 113 таких операций (46,7 % от всех исследуемых больных). Из 113 пациентов 8 пациентов умерли в послеоперационном периоде. Смертность составила 7,96 %.
В 4 случаях смерть не была напрямую связана с абсцессом головного мозга: в 1 случае больной умер от тромбоза мезентериальных артерий с развившимся перитонитом, двое больных — вследствие кровоизлияний в ложе абсцесса, причем в 1 случае — с прорывом и тампонадой желудочковой системы, и у 1 больного, по данным патологоанатомического заключения, оказался метастаз Са легкого с распадом и нагноением.
Надо отметить, что из 8 умерших больных трое находились при поступлении в коматозном состоянии (по шкале комы Глазго (ШКГ) меньше 9 баллов); четверо — в глубоком оглушении (по ШКГ 11–12 баллов) и только один в ясном сознании.
На втором месте по количеству произведенных операций — дренирование абсцесса головного мозга. Таких операций выполнено 80, что составило 33 % от всех проанализированных случаев. В 9 случаях понадобилось повторное оперативное вмешательство (11,3 %).
Из 80 пациентов в послеоперационном периоде умерло 11 пациентов. Смертность составила 13,8 %.
В 3 случаях смерть наступила от причин, не связанных с поражением головного мозга: в одном случае — в результате кровоизлияния в ложе абсцесса с прорывом в желудочковую систему, в другом — от аспирационной пневмонии, в третьем — от ятрогенного повреждения средней мозговой артерии.
Из 11 умерших пациентов 4 поступили в ясном сознании (15 баллов по ШКГ), 4 — в оглушении (11–12 баллов по ШКГ), 1 — в сопоре (10 баллов по ШКГ), 2 — в коме (меньше 9 баллов по ШКГ).
Следующий метод лечения связан с навигационными методиками. Так, с помощью безрамочной нейронавигации прооперировано 11 больных. В 5 случаях выполнено дренирование абсцессов, в 2 — пункция и аспирация содержимого абсцесса, в 4 — тотальное удаление под контролем навигации.
Десяти пациентам произведено оперативное лечение с использованием стереотаксической аспирации абсцессов головного мозга.
Нужно отметить, что при использовании навигационных методик в лечении пациентов с абсцессом головного мозга смертельных исходов не было. Однако нельзя не отметить, что на данный вид лечения пациентов отбирали более тщательным образом, чаще в плановом порядке. Так, в этой группе больных нет ни одного больного, который поступал бы в сопорозном или коматозном состоянии. 13 пациентов были в ясном сознании (по ШКГ 15 баллов), 8 — в умеренном оглушении (13–14 баллов по ШКГ).
В 1 случае дренирование оказалось неэффективным, и в последующем пациенту выполнено тотальное удаление абсцесса.
Пункционный метод без использования нейронавигационных методик, так называемый «от руки», выполнялся в 15 случаях (6,2 %). В 5 случаях понадобилась повторная пункция (30 %). В 3 случаях наступил летальный исход (смертность составила 20 %), хотя в 2 случаях он наступил у пациентов с ВИЧ-инфекцией в III клинической стадии.
Культуральные исследования содержимого абсцессов и определение чувствительности выделенных возбудителей к антибактериальным препаратам в нашем исследовании производились во всех случаях. Положительный результат получен в 58 (24,9 %) случаях. Грамположительная флора преобладала в 44 случаях, грамотрицательная — в 14. Анаэробные патогены и их комбинации, доминирующие, по многочисленным литературным данным, в этиологии абсцессов головного мозга, из-за отсутствия технических возможностей в наших лабораториях не определялись.
Состояние сознания является единственным наиболее важным фактором прогноза. Чем хуже состояние больного (по ШКГ меньше 9 баллов), тем хуже прогноз для жизни больного [30, 32, 35].
Так, Xiao и др. сообщают, что 13 пациентов (62 %) из 21 с показателем ШКГ меньше 9 баллов при поступлении либо впали в вегетативное состояние, либо умерли в послеоперационном периоде.
В нашем исследовании по уровню сознания умершие больные распределились следующим образом (табл. 1).
Выбор метода хирургического лечения абсцессов головного мозга был и остается предметом многих дебатов [24, 30, 34].
Стереотаксическая аспирация абсцесса головного мозга имеет широкое распространение с момента появления КТ. Стереотаксис позволяет точно локализовать расположение абсцесса, задать нужную, безопасную траекторию для пункции абсцесса. Стереотаксическая аспирация особенно показана для лечения абсцессов, расположенных глубинно и в функционально значимых зонах [19].
Стереотаксическая аспирация в настоящее время считается многими авторами операцией выбора при абсцессах головного мозга [5, 10, 12, 14, 21, 23].
Однако некоторые авторы отмечают и негативные стороны этого метода лечения. Так, аспирация абсцесса может привести к субарахноидальному или субдуральному вытеканию гноя [16]. Также недостатком стереотаксической аспирации является «соскальзывание» иглы при плотной капсуле абсцесса и неполной эвакуации содержимого абсцесса, что приводит к повторным пункциям. Так, Cavesoglu и др. отмечают, что у 30 из 32 пациентов производились повторные стереотаксические аспирации до двух-трех раз [11].
Mamelak сообщает, что в их исследовании 62 % пациентов подверглись повторной установке дренажа после первичной аспирации [21].
Открытое (в результате краниотомии) удаление абсцесса головного мозга также имеет своих сторонников. Так, тотальное удаление абсцесса позволяет произвести полное удаление гнойного материала и окружающей абсцесс капсулы, что может уменьшить необходимость в дополнительном лечении и сократить продолжительность антибактериальной терапии [22, 27, 36, 37, 25].
Пункционный метод лечения без нейронавигации считаем в современных условиях развития медицины нецелесообразным из-за большого количества осложнений.
В нашем исследовании при пункции «от руки» отмечались «сухие» пункции, а также из 15 случаев в повторных пункциях нуждались 5 пациентов, что составляет 30 %. При дренировании без использования нейронавигации схожая картина: в 11 % случаев требовалось повторное дренирование.
В нашем исследовании наиболее приемлемыми способами хирургического лечения были стереотаксические методы и тотальное удаление абсцессов.
При стереотаксических методах лечения смертность в нашем исследовании равна нулю. Хотя нельзя не заметить более тщательный отбор пациентов для данного вида лечения. Не было ни одного пациента с показателями ШКГ меньше 11 баллов.
Выводы
Следует подчеркнуть важность предпочтений конкретного нейрохирурга в выборе метода лечения [15], также не последнюю роль играет оснащенность операционной при выборе тактики оперативного вмешательства.
Стереотаксические методы лечения в настоящее время являются методом выбора, особенно при глубинно расположенных абсцессах и абсцессах, расположенных в функциональных зонах.
При многокамерных абсцессах, абсцессах, вызванных анаэробной флорой, при посттравматических абсцессах с наличием инородных тел, а также в клиниках с ограниченными ресурсами полное удаление абсцесса может быть подходящим методом для лечения абсцессов головного мозга.
Список литературы
1. Гайдар Б.В. Практическая нейрохирургия. — СПб.: Гиппократ, 2002. — 648 с.
2. Гринберг М.С. Нейрохирургия: Пер. с англ. — М.: МЕДпресс-информ, 2010. — 1008 с.
3. Agarwal A.K., Garg R., Simon M. Ring enhancing lesion in CT scan: metastases or a brain abscess // Emerg. Med. J. — 2007. — Vol. 24. — P. 706.
4. Alderson P.O., Gado M.H., Siegel B.A. Computerized cranial tomography and radionuclide imaging in the detection of intracranial mass lesions // Semin. Nucl. Med. — 1977. — Vol. 7. — P. 161-173;
5. Barlas O., Sencer A., Erkan K., Eraksoy H., Sencer S., Bayindir C. Stereotactic surgery in the management of brain abscess // Surg. Neurol. — 1999. — Vol. 52. — P. 404-11.
6. Beller A.J., Sahar A., Praiss I. Brain abscess. Review of 89 cases over a period of 30 years // J. Neurol. Neurosurg. Psychiatry. — 1973. — Vol. 36. — P. 757-768.
7. Bernardini G.L. Diagnosis and management of brain abscess and subdural empyema // Curr. Neurol. Neurosci. Rep. — 2004. — Vol. 4. — P. 448-456.
8. Britt R.H., Enzmann D.R. Clinical Stages of Human brain abscesses on Serial CT Scans After contrast infusion // J. Neurosurg. — 1983. — Vol. 59. — P. 72-89.
9. Calfee D.P., Wispelwey B. Brain abscess // Semin. Neurol. — 2000. — Vol. 20. — P. 353-360.
10. Carpenter J., Stapleton S., Holliman R. Retrospective analysis of 49 cases of brain abscess and review of the literature // Eur. J. Clin. Microbiol. Infect. Dis. — 2007. — Vol. 26. — P. 1-11.
11. Cavusoglu H., Kaya R.A., Turkmenoglu O.N., Colak I., Aydin Y. Brain abscess: Analysis of results in a series of 51 patients with a combined surgical and medical approach during an 11-year period // Neurosurg. Focus. — 2008. — Vol. E9. — P. 24.
12. Erdogan E., Izci Y., Gonul E., Timurkaynak E. Ventricular injury following cranial gunshot wounds: clinical study // Mil. Med. — 2004. — Vol. 169. — P. 691-695.
13. Gortvai P., De Louvois J., Hurley R. The bacteriology and chemotherapy of acute pyogenic brain abscess // Br. J. Neurosurg. — 1987. — Vol. 1. — P. 189-203.
14. Hakan T. Bacterial brain abscesses: an evaluation of 96 ca-ses // J. Infect. — 2006. — Vol. 52. — P. 359-366.
15. Hakan T. Management of bacterial brain abscesses // Neurosurg. Focus. — 2008. — Vol. E4. — P. 24.
16. Hall W.A., Truwit C.L. The surgical management of infections involving the cerebrum // Neurosurgery. — 2008. — Vol. 62. — P. 519-31;
17. Kao P.T. Brain abscess:clinical analysis of 53 cases // J. Microbiol. Immunol. Infect. — 2003. — Vol. 36, № 2. — P. 129-136.
18. Karasu A., Cansever T., Sabancı P.A., Kiris T., Imer M., Oran E. et al. Craniocerebral civilian gunshot wounds: one hospital’s experience // Ulus Travma Acil Cerrahi Derg. — 2008. — Vol. 14. — P. 59-64.
19. Kocherry X.G., Hegde T., Sastry K.V., Mohanty A. Efficacy of stereotactic aspiration in deep-seated and eloquent-region intracranial pyogenic abscesses // Neurosurg. Focus. — 2008. — Vol. E13. — P. 24.
20. Loftus C.M., Osenbach R.K., Biller J. Diagnosis and management of brain abscess // Wilkins R.H., Rengachary S.S. (eds). Neurosurgery. — 2nd ed. — New York: McGraw-Hill, 1996. — Vol. 3. — P. 3285-3298.
21. Mamelak A.N., Mampalam T.J., Obana W.G., Rosenblum M.L. Improved management of multiple brain abscesses: a combined surgical and medical approach // Neurosurgery. — 1995. — Vol. 36. — P. 76-86.
22. Mampalam T.J., Rosenblum M.L. Trends in the management of bacterial brain abscesses: A review of 102 cases over 17 years // Neurosurgery. — 1988. — Vol. 23. — P. 451-8.
23. Mathisen G.E., Johnson J.P. Brain abscess // Clin. Infect. Dis. — 1997. — Vol. 25. — P. 763-81.
24. Ng P.Y., Seow W.T., Ong P.L. Brain abscesses: review of 30 cases treated with surgery // Aust N. Z. J. Surg. — 1995. — Vol. 65. — P. 664-666.
25. Nisha Gadgil, Akash J. Patel, and Shankar P. Gopinath: Open craniotomy for brain abscess: A forgotten experience? // Surg. Neurol. Int. — 2013. — Vol. 4. — P. 34.
26. Osenbach R.K., Loftus C.M. Diagnosis and management of brain abscess // Neurosurg. Clin. N. Am. — 1992. — Vol. 3. — P. 403-420.
27. Ratnaike T.E., Das S., Gregson B.A., Mendelow A.D. A review of brain abscess surgical treatment-78 years: Aspiration versus excision // World Neurosurg. — 2011. — Vol. 76. — P. 431.
28. Roche M., Humphreys H.E., Phillips J., Cunney R., McNamara E. et al. A twelve-year review of central nervous system bacterial abscesses; presentation and aetiology // Clin. Microbiol. Infect. — 2003. — Vol. 9. — P. 803-809.
29. Salzman C., Tuazon C.U. Value of the ring-enhancing sign in differentiating intracerebral hematoms and brain abscess // Arch. Intern. Med. — 1987. — Vol. 147. — P. 951-952.
30. Sharma B.S., Gupta S.K., Khosla V.K. Current concepts in the management of pyogenic brain abscess // Neurol. India. — 2000. — Vol. 48. — P. 105-111.
31. Stapleton S.R., Bell B.A., Uttley D. Stereotactic aspiration of brain abscesses: is this the treatment of choice? // Acta Neurochir. — 1993. — Vol. 121. — P. 15-19.
32. Takeshita M., Kagawa M., Izawa M., Takakura K. Current treatment strategies and factors influencing outcome in patients with bacterial brain abscess // Acta Neurochir. (Wien). — 1998. — Vol. 140. — P. 1263-1270.
33. Tattevin P. Bacterial brain abscess // Am. J. Med. — 2003. — Vol. 115, № 2. — P. 143-146.
34. Wise B.L., Gleason C.A. CT-directed stereotactic surgery in the management of brain abscess // Ann. Neurol. — 1979. — Vol. 6. — P. 457.
35. Xiao F., Tseng M.Y., Teng L.J., Tseng H.M., Tsai J.C. Brain abscess: clinical experience and analysis of prognostic factors // Surg. Neurol. — 2005. — Vol. 63. — P. 442-450.
36. Yang S.Y. Brain abscess: A review of 400 cases // J. Neurosurg. — 1981. — Vol. 55. — P. 794-799.
37. Yang S.Y., Zhao C.S. Review of 140 patients with brain abscess // Surg. Neurol. — 1993. — Vol. 39. — P. 290-296.

-vak/29-1.jpg)
-vak/30-1.jpg)
-vak/31-1.jpg)