Статья опубликована на с. 61-65
Одним из основных факторов, влияющих на прогноз пациентов, перенесших инфаркт миокарда (ИМ), является размер некроза сердечной мышцы [17]. В связи с этим особую настороженность вызывает выживаемость больных, перенесших бивентрикулярный ИМ [16]. Инфаркт миокарда правого желудочка (ПЖ) наблюдается при Q-ИМ задней стенки (ЗС) левого желудочка (ЛЖ) в 30–50 % случаев, хотя в ряде литературных источников указывается более значительная вариабельность частоты (14–84 %), что в первую очередь свидетельствует о недостаточной настороженности в выявлении правожелудочкового повреждения при Q-ИМ ЗС ЛЖ [10, 14]. На сегодняшний день не сформировано единого мнения о вкладе ИМ ПЖ в ближайший и отдаленный прогноз больных [13]. Ряд исследователей объясняют увеличение риска фатальных осложнений не столько с фактом инфарцирования ПЖ, сколько с обширностью некроза ЛЖ [7]. С другой стороны, ряд убедительных данных свидетельствует о непосредственном влиянии инфаркта ПЖ на увеличение смертности и фатальных осложнений как в остром периоде, так и в долгосрочной перспективе [8, 10, 16].
В связи с этим выявление дополнительных маркеров риска, которые могли бы расширить возможности стратификации раннего и отдаленного прогноза больных с ИМ ПЖ, не теряет своей значимости.
В качестве надежного инструмента ранней диагностики ИМ, оценки риска и терапевтического мониторинга широкое распространение в клинике получило использование биологических маркеров [5]. В последние годы предметом научного интереса является исследование клинической роли галектина-3 — представителя семейства β-галактозидсвязывающих протеинов, который принимает участие в многочисленных физиологических и патологических процессах, включая межклеточное взаимодействие, рост клетки, неопластическую трансформацию, стимуляцию апоптоза, ангиогенеза, индукцию воспаления и фиброза [3, 11].
Результаты клинических испытаний доказали возможность использования серийного исследования галектина-3 в качестве маркера риска осложнений у больных с острой и хронической сердечной недостаточностью (СН) [12, 15]. Ряд научных исследований указывает на тесную связь галектина-3 с развитием неблагоприятных клинических последствий у больных с острым коронарным синдромом (ОКС) [6, 9]. Однако прогностическая роль галектина-3 совсем не изучалась у больных с ИМ ПЖ, что повышает клинический интерес к этому вопросу.
Цель работы: оценить прогностическую значимость галектина-3 в формировании комбинированной конечной точки при 30-месячном наблюдении у пациентов, перенесших инфаркт миокарда правого желудочка на фоне Q-инфаркта миокарда задней стенки левого желудочка.
Материалы и методы
Обследовано 155 больных, которые находились на лечении в кардиологическом отделении Сумской городской клинической больницы № 1 в период с декабря 2010 по июнь 2014 г. с диагнозом «острый Q-ИМ ЗС ЛЖ с вовлечением ПЖ». Возраст пациентов — от 34 до 83 лет (64,11 ± 0,78 года), из них было 103 (66,5 %) мужчины и 52 (33,5 %) женщины.
Острый Q-ИМ ЗС ЛЖ и инфарцирование ПЖ диагностировали на основании клинического и лабораторно-инструментального обследований в соответствии с рекомендациями Европейского общества кардиологов (2012 г.) [17].
Стадию СН по Стражеско — Василенко и функциональный класс (NYHA) устанавливали в соответствии с рекомендациями Украинского общества кардиологов (2012 г.) [1].
Уровень галектина-3 определяли на 2-е сутки ИМ и через 6 месяцев в сыворотке венозной крови больных методом твердофазного иммуноферментного анализа с использованием набора реактивов Human Galectin-3 Platinum ELISA (Vienna, Austria).
Общий период наблюдения составил 30,6 ± 4,5 месяца. Оценивали комбинированную конечную точку, которая включала сердечно-сосудистую смерть, нестабильную стенокардию (НС), повторный ИМ и острые нарушения мозгового крово–обращения (ОНМК). Эти осложнения были зарегистрированы у 62 (40 %) больных с постинфарктным кардиосклерозом на фоне ИМ ПЖ и ЗС ЛЖ, что объединило этих пациентов в группу с осложненным течением (1-я группа). У 93 (60 %) человек пост–инфарктный период в течение 30 месяцев протекал относительно благоприятно (2-я группа).
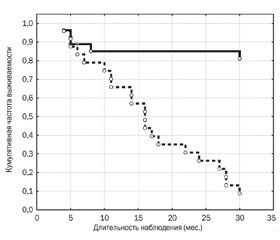
Статистическую обработку полученных данных проводили с помощью пакета статистических программ Statistica 8.0 (StatSoft Inc., США) с использованием непараметрического критерия Манна — Уитни. Достоверность результатов оценивали по t-критерию Стьюдента для зависимых и независимых выборок. Для сравнения качественных характеристик использовали критерий χ2 Пирсона (при малой выборке с поправкой Йетса). Для выявления связи между показателями и оценки относительного вклада каждой независимой переменной использовали многофакторный регрессионный анализ с расчетом стандартизованных регрессионных коэффициентов. Оценку кумулятивной доли пациентов без конечных точек проводили путем построения таблиц дожития с графическим изображением методом Каплана — Мейера с использованием модели Кокса. Для всех видов анализа отличия считали статистически достоверными при р < 0,05.
Результаты и обсуждение
По результатам 30-месячного периода наблюдения комбинированная конечная точка исследования была достигнута у 62 (40 %) пациентов — 1-я группа. Зарегистрировано 50 (32,2 %) случаев повторных госпитализаций по поводу НС, повторный ИМ перенесли 15 больных (9,6 %), ОНМК — 9 (5,8 %) обследованных. В ходе наблюдения по сердечно-сосудистым причинам умерло 14 человек (6,4 %).
На момент включения в исследование группы пациентов с осложненным течением постинфарктного периода и без осложнений не отличались по гендерному признаку, количеству курильщиков и частоте употребления алкоголя.
Исходные данные 1-й группы больных характеризовались старшим возрастом (67,70 ± 0,95 года, р = 0,0001), большей продолжительностью анамнеза ИБС (в 2,3 раза, р < 0,0001) и количеством перенесенных ОНМК (24,2 %, р = 0,0145) и ИМ (в 3 раза, р = 0,002). В перечне сопутствующей патологии у них достоверно чаще диагностировали сахарный диабет (СД) (38,7 %, р = 0,0156), артериальную гипертензию (АГ) (91,9 %, р = 0,026) и периферический атеросклероз нижних конечностей (25,8 %, р = 0,0037) (табл. 1).
Галектин-3 играет роль посредника в межклеточном взаимодействии. Для него характерны многочисленные аутокринные и паракринные свойства, он усиливает провоспалительные сигналы, обладая хемотаксической функцией по отношению к макрофагам и моноцитам, регулирует процессы апоптоза, фиброза и ангиогенеза, что объясняет его участие в процессах атерогенеза, прогрессирования сердечной недостаточности и дестабилизации атеросклеротической бляшки [2, 9].
Концентрация галектина-3 на 2-е сутки острого ИМ ПЖ определялась в диапазоне 18,8–42,9 нг/мл (31,48 ± 0,79 нг/мл), при этом средние значения галектина-3 в 1-й группе были достоверно выше показателей пациентов с благоприятным течением пост–инфарктного периода (35,61 ± 0,64 нг/мл против 26,83 ± 0,72 нг/мл, р < 0,0001) (табл. 3).
В результате многофакторного регрессионного анализа было установлено, что уровень галектина-3, определенный на 2-е сутки ИМ ПЖ, был независимым фактором риска нестабильной стенокардии, повторных ИМ и сердечно-сосудистой смертности в последующие 30 месяцев наблюдения (табл. 2).
При повторном исследовании через 6 месяцев после ИМ ПЖ колебания уровня галектина-3 составляли 14,2–60,1 нг/мл, в среднем — 29,28 ± 1,77 нг/мл, что достоверно не отличалось от исходных значений (р = 0,262) (табл. 3). В группе пациентов с осложненным течением постинфарктного периода средний уровень галектина-3 составлял 38,61 ± 2,04 нг/мл, р < 0,0001, что достоверно превышало показатель больных 2-й группы — 18,8 ± 0,53 нг/мл, р < 0,0001. В динамике наблюдения было установлено, что в группе пациентов с осложнениями в постинфарктном периоде уровень галектина-3 через 6 месяцев несколько увеличился (38,61 ± 2,04 нг/мл, р = 0,17), в то же время у больных с отсутствием осложнений он достоверно уменьшился и составлял 18,80 ± 0,53 нг/мл (р < 0,0001) (табл. 3).
Показатели галектина-3, полученные в данном исследовании, соответствуют высоким значениям. Данные литературы указывают, что у пациентов с ОКС средние значения галектина-3 (16,7 нг/мл) ассоциируются с 2-кратным увеличением риска прогрессирования СН по сравнению с показателем 14,6 нг/мл [9]. В исследовании C.R. de Fillipi и соавт. (2010 г.) среднее нормальное значение галектина-3 у лиц без признаков СН соответствовало уровню 1,092 нг/мл. У пациентов с СН смертность в течение года в нижнем квартиле галектина-3 (< 12,0 нг/мл) составляла 10,3 % и увеличивалась до 32,5 % при концентрации галектина-3, превышающей значения 22,3 нг/мл [4].
Пошаговый многофакторный регрессионный анализ продемонстрировал, что уровень галектина-3, определенный через 6 месяцев после ИМ ПЖ, был достоверно и независимо связан с развитием сердечно-сосудистых осложнений — повторными ИМ, нестабильной стенокардией, ОНМК и сердечно-сосудистой смертностью — на протяжении 30-месячного периода наблюдения (табл. 4).
Эти данные находят подтверждение в результатах исследования C. Falcone, S. Lucibello, I. Mazzucchelli еt al. (2011 г.), которые не только продемонстрировали связь галектина-3 с наличием 1–2 сосудистых атеросклеротических поражений коронарных артерий, но и показали достоверное увеличение галектина-3 при развитии клиники нестабильной стенокардии. Авторы указали на целесообразность использования галектина-3 в качестве маркера дестабилизации атеросклеротической бляшки и развития ОКС [6].
Результаты 30-месячного наблюдения за пациентами, перенесшими ИМ ПЖ на фоне Q-ИМ ЗС ЛЖ, показали наличие прямой связи между концентрацией галектина-3, определенной через 6 месяцев после ИМ ПЖ, и частотой развития комбинированной конечной точки. Кривые выживания Каплана — Мейера распределены в зависимости от наличия у больных комбинированной конечной точки при концентрации галектина-3 выше или ниже среднего значения (29,28 нг/мл) на момент 6 месяцев после ИМ ПЖ.
В исследовании PROVE IT-TIMI 22 было показано, что у пациентов, перенесших острый коронарный синдром, уровень галектина-3, определенный на 7-е сутки, является независимым маркером патологического ремоделирования миокарда и предиктором прогрессирования сердечной недостаточности [9]. Результаты данного исследования также продемонстрировали прогностическое значение галектина-3 у больных с ИМ ПЖ в развитии жизненно опасных осложнений и сердечно-сосудистой смерти в отдаленном периоде инфаркта.
Выводы
1. Доказано прогностическое значение галектина-3 в развитии сердечно-сосудистых осложнений на протяжении 30 месяцев наблюдения у больных с ИМ ПЖ на фоне Q-ИМ ЗС ЛЖ.
2. Показана связь между высокой концентрацией галектина-3, определенной через 6 месяцев после ИМ ПЖ, с частотой комбинированной сердечно-сосудистой точки по итогам 30-месячного наблюдения.
Список литературы
1. Воронков Л.Г., Амосова К.М., Багрій А.Е. та ін. Рекомендації з діагностики та лікування хронічної серцевої недостатності // Серцева недостатність. — 2012. — № 3. — С. 60-96.
2. De Boer R.A., Voors A.A., Muntendam P. Galectin-3: a novel mediator of heart failure development and progression // European Journal of Heart Failure. — 2009. — Vol. 11. — P. 811-817.
3. Calvier L. Miana M., Reboul P. et al. Galectin-3 mediates aldosterone-induced vascular fibrosis // Atheroscler. Thromb. Vasc. Biol. — 2013. — Vol. 33 — P. 67–75.
4. DeFilippi C., Felker M. Galectin-3 in Heart Failure — Linking Fibrosis, Remodeling and Progression // US Cardiology. — 2010. — Vol. 7(1). — P. 67-70.
5. Doehner W. Diagnostic biomarkers in cardiovascular di–sease. Diagnostic biomarkers in cardiovascular disease: the proteomics approach // Eur. Heart J. — 2012. — Vol. 33. — № 18. —
P. 2317-2324.
6. Falcone C., Lucibello S., Mazzucchelli I. et al. Galectin-3 plasma levels and coronary artery disease: a new possible biomarker of acute coronary syndrome // J. Immunopathol. Pharmacol. — 2011. — Vol. 24. — Vol. 4. — P. 905-913.
7. Halkin A., Singh M., Nikolsky E., et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction. The Cardillak Risk Score // J. Am. Coll. Cardiol. — 2005. — Vol. 45. — P. 1397-1405.
8. Hamon M., Agostini D., Page O. et.al. Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: Meta-analysis // Crit. Care Med. — 2008. — Vol. 36. — P. 2023-2033.
9. Grandin E.W., Jarolim P., Ritterowa L. et al. Galectin-3 and the development of heart failure after acute coronary syndrome: a pilot experience from PROVE IT-TIMI 22 // Clinical Chemistry. — 2012. — Vol. 58. — P. 267-273.
10. Jensen C.J., Jochims M., Hunold P. et al. Right ventricular involvement in acute left ventricular myocardial infarction: prognostic implications of MRT findings // AJR. — 2010. — Vol. 194. — P. 592-598.
11. Kramer F. Galectin-3: clinical utility and prognostic value in patients with heart failure // Reasearch Reports in Clinical Cardio–logy. — 2013. — Vol. 4. — P. 13-22.
12. Lok D., Van Der Meer, Porte P. et al. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study // Clin. Res. Cardiol. — 2010. — Vol. 99. — P. 323–328.
13. Ninkovic V., Perunicic J., Ninkovic S. et al. Predictors of In-Hospital Mortality in Patients with Acute Inferior Infarction of the Left Ventricle Accompanied by Right Ventricular Infarction when Treated with Percutaneous Coronary Intervention // J. Clin. Exp. Cardiolog. — 2013. — Vol. 4. — P. 253-258.
14. Pereira A., Franken R., Sproviery SR et al. Impact on hospital mortality and morbidity of right ventricular involvement among patients with acute left ventricular infarction // Sao Paulo Med J. — 2006. — Vol. 124(4). — P. 186-191.
15. Shan R.V., Chen-Tournoux A.A., Picard M.H. et al. Galectin-3, cardiac structure and function, and long-term mortality in patients with acute decompensated heart failure // Eur. J. Heart Fail. — 2010. — Vol. 12(8). — P. 826-832.
16. Stanley G., Mansi P., Ashok T. Clinical profile and in-hospital outcome of patients with right ventricular myocardial infarction // International Journal of Clinical Medicine. — 2014. — Vol. 5. — P. 459-463.
17. Steg G., James S., Atar D. et al. ESC Guidelines for the ma–nagement of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the management of –ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) // European Heart Journal. — 2012. — Vol. 33. — P. 2569-2619.
1. Voronkov L.H., Amosova K.M., Bahriy A.E. ta in. Rekomendatsiyi z diahnostyky ta likuvannya khronichnoyi sertsevoyi nedostatnosti (2012) // Sertseva nedostatnist'. — 2012. — #3. — S. 60-96.
2. De Boer RA, Voors AA, Muntendam P, van Gilst WH, van Veldhuisen DJ. Galectin-3: a novel mediator of heart failure development and progression. European Journal of Heart Failure 2009;11:811-817. doi:10.1093/eurjhf/hfp097.
3. Calvier L, Miana M, Reboul P, Cachofeiro V, Martinez-Martinez E, de Boer RA, Poirier F, Lacolley P, Zannad F, Rossignol P, López-Andrés N. Galectin-3 mediates aldosterone-induced vascular fibrosis. Arterioscler Thromb Vasc Biol. 2013;33(1):67-75. doi: 10.1161/ATVBAHA.112.300569.
4. DeFilippi C., Felker M. Galectin-3 in Heart Failure — Linking Fibrosis, Remodeling and Progression. US Cardiology2010;7(1):67-70.
5. Doehner W. Diagnostic biomarkers in cardiovascular disease. Diagnostic biomarkers in cardiovascular disease: the proteomics approach. Eur. Heart J. 2012; 33:2317-2324. Doi:org/10.1093/eurheartj/ehs244.
6. Falcone C, Lucibello S, Mazzucchelli I, Bozzini S, D'Angelo A, Schirinzi S, Totaro R, Falcone R, Bondesan M, Pelissero G. Galectin-3 plasma levels and coronary artery disease: a new possible biomarker of acute coronary syndrome. Int J Immunopathol Pharmacol. 2011;24(4):905-13.
7. Halkin A, Singh M, Nikolsky E, Grines CL, Tcheng JE, Garcia E, Cox DA, Turco M, Stuckey TD, Na Y, Lansky AJ, Gersh BJ, O’Neilli WW, Mehran R, Stone GW. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction. The Cardillak Risk Score. J Am CollCardiol. 2005;45 (9):1397 — 1405. doi:10.1016/j.jacc.2005.01.041
8. Hamon M, Agostini D, Page O, RiddellJW, Hamon M.l. Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: Meta-analysis. Crit Care Med. 2008;36 (7):2023–2033. doi: 10.1097/CCM.0b013e31817d213d.
9. Grandin EW, Jarolim P, Murphy SA, Ritterova L, Cannon CP, Braunwald E, Morrow DA. Galectin-3 and the development of heart failure after acute coronary syndrome: a pilot experience from PROVE IT-TIMI 22. Clinical Chemistry 2012;58:267-273. Doi: 10.1373/clinchem.2011.174359.
10. Jensen CJ, Jochims M, Hunold P, Sabin GV, Schlosser T, Bruder O. Right ventricular involvement in acute left ventricular myocardial infarction: prognostic implications of MRT findings. AJR Am J Roentgenol. 2010 Mar;194(3):592-8. doi: 10.2214/AJR.09.2829.
11. Kramer F. Galectin-3: clinical utility and prognostic value in patients with heart failure. Reasearch Reports in Clinical Cardiology 2013;4:13-22. Doi: 10.2147/RRCC.S28562
12. Lok DJA, Van Der Meer P, de la Porte PW B-A, Lipsis E, Van Wijngaarden J. Prognostic value of galectin-3, a novel marker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 2010;99:323–328. Doi:10.1007/s00392-010-0125-y.
13. Ninkovic VM, Perunicic JZ, Ninkovic SM, Miloradowic VM, Vojislav G, Jakovljevic DG. Predictors of In-Hospital Mortality in Patients with Acute Inferior Infarction of the Left Ventricle Accompanied by Right Ventricular Infarction when Treated with Percutaneous Coronary Intervention . J Clin Exp Cardiolog 2013;4: 253-258. Doi:10.4172/2155-9880.1000253
14. Pereira A., Franken R., Sproviery SR, Golin V. Impact on hospital mortality and morbidity of right ventricular involvement among patients with acute left ventricular infarction // Sao Paulo Med J. 2006;124(4):186-191.
15. Shan RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL. Galectin-3, cardiac structure and function, and long-term mortality in patients with acute decompensated heart failure // Eur J Heart Fail. 2010 August; 12(8): 826–832. doi: 10.1093/eurjhf/hfq091
16. Stanley G, Mansi P, Ashok T. Clinical profile and in-hospital outcome of patients with right ventricular myocardial infarction. International Journal of Clinical Medicine 2014;5:459-463. Doi: 10.4236/ijcm.2014.58064.
17. Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K,Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van 't Hof A, Widimsky P, Zahger D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Eur Heart J. 2012 Oct;33(20):2569-619. doi: 10.1093/eurheartj/ehs215.

/63-1.jpg)
/64-1.jpg)
/64-2.jpg)