Резюме
Myasthenic crisis may be defined as respiratory failure or delayed extubation after surgical treatment for more than 24 hours resulting from myasthenic weakness. Myasthenic crisis results from weakness of upper airway muscles leading to obstruction and aspiration, weakness of respiratory muscles leading to reduced tidal volumes, or weakness of both muscle groups. About 1/5 of patients with myasthenia gravis experience crisis, usually within the first year of illness. Over the last four decades, prognosis from myasthenic crisis has dramatically improved from a mortality rate of 75 % to the current rate of less than 5 %. Myasthenic crisis should not be fatal, as long as patients receive timely respiratory support and appropriate immunotherapy to reduce myasthenic weakness of the respiratory muscles. In the last years there are more reports about the development of urgent conditions in patients with myasthenia gravis in the early postoperative period after thymectomy. Long-term follow-up monitoring for the study effects of thymectomy in patients with myasthenia gravis, conducted in the department of thoracic surgery of State Institution «Institute of General and Emergency Surgery named after V.T. Zaitsev of National Academy of Medical Sciences of Ukraine» showed that the incidence of early postoperative myasthenic crisis amounted 9.2–12.3 % of cases and was associated with the degree of compensation of bulbar and respiratory disorders before the surgery. This reflects the importance of an adequate selection of the dose of anticholinesterase drugs in the preoperative stage for effective compensation neurosomatic disorders and favorable postoperative prognosis. As an example, the complicated course of generalized myasthenia gravis after thymthymomectomy was described.
Миастенические кризы — состояния, при которых возникает дыхательная недостаточность или задержка экстубации после хирургического лечения более чем на 24 часа вследствие миастенической слабости. Данные неотложные состояния являются результатом слабости мышц верхних дыхательных путей, приводя к обструкции и аспирации, слабости дыхательной мускулатуры, что, в свою очередь, обусловливает уменьшение дыхательного объема или слабость обеих мышечных групп. Примерно у 1/5 пациентов с миастений наблюдаются кризовые состояния, обычно на первом году заболевания. За последние сорок лет прогноз при миастеническом кризе значительно улучшился: уровень смертности понизился с 75 % до нынешнего показателя в менее чем 5 %. Миастенический криз не должен иметь летальный исход, если пациенты получают своевременную респираторную поддержку и соответствующую иммунотерапию с целью уменьшения миастенической слабости дыхательной мускулатуры. В последние годы появляется все больше сообщений о развитии кризовых состояний у пациентов с миастенией в раннем послеоперационном периоде после тимэктомии. Длительное катамнестическое наблюдение по изучению эффектов тимэктомии у больных с миастенией, проведенное в торакальном отделении ГУ «Институт общей и неотложной хирургии им. В.Т. Зайцева НАМН Украины», показало, что частота развития миастенических кризов в раннем послеоперационном периоде составляла 9,2–12,3 % случаев и была связана со степенью компенсации бульбарных и дыхательных нарушений перед хирургическим вмешательством. Это отражает важность адекватного подбора дозы антихолинэстеразных препаратов на предоперационном этапе для эффективной компенсации нейросоматических расстройств и благоприятного послеоперационного прогноза. В качестве примера приведен клинический случай осложненного течения генерализованной миастении после тимтимомэктомии.
Мiастенiчнi кризи — стани, при яких виникає дихальна недостатність або затримка екстубації після хірургічного лікування більше ніж на 24 години внаслiдок міастенічної слабкості. Ці невідкладні стани є результатом слабкості м’язів верхніх дихальних шляхів, приводячи до обструкції та аспірації, слабкості дихальної мускулатури, що, у свою чергу, зумовлює зменшення дихального об’єму або слабкість обох м’язових груп. Приблизно в 1/5 пацієнтів iз міастенією спостерігаються кризовi стани, зазвичай на першому році захворювання. За останні сорок років прогноз при міастенічному кризі значно покращився: рівень смертності знизився з 75 % до нинішнього показника в менше ніж 5 %. Міастенічний криз не повинен мати летальний кінець, якщо пацієнти отримують своєчасну респіраторну підтримку і відповідну імунотерапію з метою зменшення міастенічної слабкості дихальної мускулатури. В останні роки з’являється все більше повідомлень про розвиток кризових станів у пацiєнтiв iз міастенією в ранньому післяопераційному періоді після тимектомії. Тривале катамнестичне спостереження з вивчення ефектів тимектомії у хворих на міастенію, проведене в торакальному відділенні ДУ «Інститут загальної та невідкладної хірургії ім. В.Т. Зайцева НАМН України», показало, що частота розвитку міастенічних кризів у ранньому післяопераційному періоді становила 9,2–12,3 % випадків і була пов’язана зі ступенем компенсації бульбарних і дихальних порушень перед хірургічним втручанням. Це відображає важливість адекватного підбору дози антихолінестеразних препаратів на передопераційному етапі для ефективної компенсації нейросоматичних розладів і сприятливого післяопераційного прогнозу. Як приклад наведено клінічний випадок ускладненого перебігу генералізованої міастенії після тимтимомектомії.
The article was published on p. 46-49
Myasthenic crisis may be defined as respiratory failure or delayed extubation after surgical treatment for more than 24 hours resulting from myasthenic weakness. Myasthenic crisis results from weakness of upper airway muscles leading to obstruction and aspiration, weakness of respiratory muscles leading to reduced tidal volumes, or from weakness of both muscle groups [1–5].
About one-fifth of patients with myasthenia gravis experience crisis, usually within the first year of illness. Over the last four decades, prognosis from myasthenic crisis has dramatically improved from a mortality rate of 75 % to the current rate of less than 5 %. Common precipitating factors for myasthenic crisis include respiratory infections, aspiration, sepsis, surgical procedures, rapid tapering of immune modulation, beginning treatment with corticosteroids, exposure to drugs that may increase myasthenic weakness, and pregnancy. Myasthenic crisis should not be fatal, as long as patients receive timely respiratory support and appropriate immunotherapy to reduce myasthenic weakness of the upper airway and respiratory muscles [1, 2].
Emergency conditions in myasthenia gravis are divided into:
— myasthenic crisis;
— cholinergic crisis;
— mixed crisis.
Myasthenic crisis is suddenly developed critical condition in patients with myasthenia, which shows not only quantitative but also a qualitative change in the nature of the process. Pathogenesis of crisis due not only to a decrease in the density of cholinergic receptors of postsynaptic membrane as a result of complement-mediated destruction of them. But with a change in the functional state of the remaining receptors and ion channels [1].
Initially, breathing becomes frequent, shallow, with the inclusion of accessory muscles, and then — a rare, intermittent. Further the phenomenon of hypoxia is developed. Join anxiety and agitation. Develop motor restlessness, followed by a full stop breathing, confusion and loss of consciousness. Violation of cardiovascular activity at the time of crisis is expressed in increased heart rate to 150–180 per minute and an increase in blood pressure [1–4].
Severe generalized myasthenic crisis manifested varying levels of loss of consciousness, severe bulbar disorders increasing respiratory failure, severe weakness of the skeletal muscles. Respiratory disorders are progressing for hours, sometimes — minutes. In the future, the pressure is reduced; the pulse becomes tense at first, then arrhythmic, rare, filamentary. Amplify vegetative symptoms — salivation, sweating. At the extreme gravity of the loss of consciousness is accompanied by involuntary urination and defecation [1–3].
Cholinergic crisis is a state that has a special mechanism for the development, due to excessive activation of the nicotinic cholinergic and muscarinic receptors due to an overdose of anticholinesterase drugs (ACED). This type of crisis, along with the development of generalized muscle weakness, is formed the whole complex by cholinergic effects [1, 3–5].
At the core of the motor and autonomic disorders in cholinergic crisis lies postsynaptic membrane hyperpolarization and cholinergic receptor desensitization, which is associated with severe blockage of acetylcholine and consequent excessive entering of acetylcholine to receptors of the postsynaptic membrane. Cholinergic crises are rare (3 % of patients) and develop more slowly than myasthenic crisis. In all cases, the appearance of them is associated with an overdose of ACED [1–4].
Within a day or a few days, the condition of patients becomes severe, increases weakness and fatigue, the patient needs to use ACED more often than has been recommended by a doctor, appear some signs of cholinergic poisoning, and then, after another injection or enteral receiving ACED (at the height of their actions — usually through 30–40 minutes), develops the picture of crisis is simulating myasthenic disorders [1, 2].
Mixed crisis occurs most frequently in clinical practice. The difficulty of its diagnosis lies in the fact that it combines all of the clinical features of myasthenic and cholinergic crisis described above. This is the worst version of vital disorders in patients with myasthenia gravis [1–4].
On the one hand, the patient needs immediate reception of ACED and on the other — it cannot tolerate the drugs and his condition is deteriorating to the background of their application. A thorough analysis of patients with mixed crisis showed that 25 % of them had already identified myasthenic and cholinergic crisis [1–5].
In the last years there are more reports about the development of urgent conditions in patients with myasthenia gravis in the early postoperative period after thymectomy. Long-term follow-up monitoring for the study effects of thymectomy in patients with myasthenia gravis, conducted in the department of thoracic surgery of State Institution «Institute of General and Emergency Surgery named after V.T. Zaitsev of National Academy of Medical Sciences of Ukraine» showed that the incidence of early postoperative myasthenic crisis amounted 9.2–12.3 % of cases and was associated with the degree of compensation of bulbar and respiratory disorders before the surgery. This reflects the importance of an ade–quate selection of the dose of ACED in the preoperative stage for effective compensation neurosomatic disorders and favorable postoperative prognosis [5, 6].
Also has been featured greater effectiveness of thymectomy in terms of myasthenic disorders remission in patients with onset before 40 years and without thymoma (in 46.2 % of cases). At the same time, the frequency of remission myasthenia gravis combined with thymoma after removal of the tumor did not exceed 34.1 % [5].
Herewith insufficient effect or absence of remission with the necessity of continuous use of corticosteroids and AСED after surgery in patients occurs much more frequently (82 %) compared with patients without thymoma (29 %). Severe myasthenic crises occurred more frequently in patients with generalized myasthenia and crises mild and moderate — at the local forms of the disease [5, 6].
One of the causes of myasthenic crisis in the postoperative period can be traumatization of operational substrate, which leads to an increase in symptoms of myasthenia gravis and, ultimately, the development of myasthenic crisis. Another cause of emergency conditions in the postoperative period is considered a sharp decrease in the number of acetylcholine receptors because of their massive attack by autoantibodies [5, 6].
As an example of a complicated course of generalized myasthenia gravis after thymthymomectomy, we describe the following observation.
Patient K. 57 years old, was admitted to the department of thoracic surgery of State Institution «Institute of General and Emergency Surgery named after V.T. Zaitsev of National Academy of Medical Sciences of Ukraine» with complaints of periodically weakness in the muscles of the shoulder, double vision, fatigue. These complaints were noted over the past year, increasing after physical activity and stressful situation. The patient was examined and treated by a neurologist on a residence, took metabolic therapy, which has led to a temporary positive effect. When conducting electroneuromyography, information about violation of neuromuscular transmission has not been identified. After computed tomography scan of mediastinum thymoma was found (dimensions 25 × 49 × 50 mm).
During clinical neurological examination of the patient a transient diplopia, diffuses decrease in the muscle tone, more pronounced in the upper extremities, and reduced muscle strength in the upper extremities to 3.5–4 points, in the lower extremities — to 4 points was found. It is corresponding to II functional class according to the classification of The Myasthenia Gravis Foundation of America (MGFA, 2001). The test with neostigmine was weakly positive. We decided to hold the surgical treatment [7].
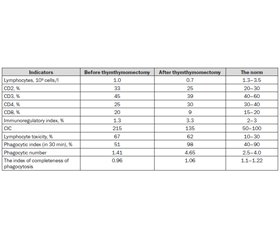
Immunological examination revealed violation of ratio subpopulations of immune cells, which was confirmed by increased levels of CD2 in combination with a reduction in the subpopulation of T-helper lymphocytes CD4 and immunoregulatory index (IRI) on the background of a minor lymphocytopenia (see Table 1). Has also been observed violation of phagocytic function that was confirmed by the decline of phagocytic number (PN) and index of completeness of phagocytosis (ICP). Incomplete phagocytic function of neutrophils and opposite changes of the intensity of the expression of cell differentiation CD clusters contributed to the accumulation of infectious antigens in tissue depots, followed by intensive formation of autoantibodies to tissue and cell organelles [6]. This is confirmed by the increase of more than 2 times the level of circulating immune complexes (CIC) in the blood of lymphocyte toxicity (see Table 1).
/48.jpg)
Was performed thymthymomectomy. After operation the symptomatic treatment (neostigmine 1.0 ml intramuscularly 4 times a day) was prescribed. In the 1st day after the operation the patient noted absence of diplopia. However, muscle weakness remained at the same level (II functional class according to the classification MGFA). On the 2nd day after surgery the state of the patient rapidly became severe, muscle strength decreased to 2 points, have joined the weakness of the respiratory muscles and respiratory failure, indicating that the development of the myasthenic crisis and the severity of the condition corresponds to V functional class according to the classification MGFA. The patient was transferred to the artificial lung ventilation [7, 8].
Immunological study of blood during the crisis has detected: lymphopenia, reduced subpopulations CD2 by 24.2 %, CD3 by 13.3 %, CD8 by 55 %, increased levels of CD4 by 20 % and IRI by 2.6 times in comparison with those prior to surgery. There was a more increase compared with those before surgery phagocytic index by 1.9 times and the PN by 3.3 times at less significant increase in the ICP, whose figure remained below the reference values.
According to European guidelines for the management of patients with myasthenia gravis (2010), for the treatment of emergency condition of the patient was prescribed a course of membrane exchange plasmapheresis [8]. Multiplicity of procedures was 3 sessions with an interval of 1 day. Number of remote plasma was 743 grams for 1 session.
As a result of the therapy the patient‘s condition has improved — to restore respiratory function, muscle strength in the limbs increased to 3.5 points (II functional class classification MGFA). After a course of exchange plasmapheresis patient he was appointed kalimin 60 mg twice a day and dexamethasone 4 mg 3 times a day with the subsequent reduction in dosage. As a result of treatment (2 weeks), muscle strength increased to 4.5 points and in a satisfactory condition the patient was discharged from the clinic.
Taking into account our findings, further detailed study of the clinical and immunological correlations in various forms of myasthenia gravis and pathology of the thymus allow to identify new ways of interaction of pathological processes, improve the outcome of surgical treatment of myasthenia gravis.
Список литературы
1. The myasthenic patient in crisis: an update of the management in Neurointensive Care Unit [Електронний ресурс] / D.A. Godoy, L.J. Vaz de Mello, L. Masott, M.D. Napoli // Arq. Neuropsiquiatr. — 2013. — Режим доступу до ресурсу: http://www.scielo.br/pdf/anp/v71n9A/0004-282X-anp-71-09-627.pdf. DOI: 10.1590/0004-282X20130108.
2. Myasthenic crisis. Clinical features, mortality, complications, and risk factors for prolonged intubation / [C.E. Thomas, S.A. Mayer, Y. Gungor et al.] // Neurology. — 1997. — Vol. 48, № 5. — P. 1253-1260. PMID: 9153452.
3. Regulatory and pathogenic mechanisms in human autoimmune myasthenia gravis / R. Le Panse, G. Cizeron-Clarac, M. Cuvelier [et al.] // Ann. N-Y. Acad. Sci. — 2008. — № 1132. — Р. 135-142. DOI: 10.1196/annals.1405.019.
4. Клинический случай миастенического криза: возможные механизмы развития, особенности клинического течения и тактика ведения / [А.Г. Санадзе, Е.К. Сепп, Н.И. Щербакова и др.] // Неврологический журнал. — 2010. — № 3. — С. 35-41.
5. Клиническая оценка характера миастенических кризов в раннем послеоперационном периоде после тимэктомии / В.В. Бойко, П.Е. Нечитайло, А.Г. Краснояружский, Ю.А. Бачерикова // Харківська хірургічна школа. — 2013. — № 4. — С. 50-53.
6. Особенности иммунофизиологических реакций у больных при различных клинических типах миастении / Е.М. Климова [и др.] // Харківська хірургічна школа. — 2014. — № 3 (66). — С. 46-52.
7. EFNS/ENS Guidelines for the treatment of ocular myasthenia / E. Kertya, A. Elsaisa, Z. Argovc [et al.] // European Journal of Neurology. — 2014. — № 2. — Р. 687-693. DOI: 10.1111/ene.12359.
8. Therapeutic plasma exchange in the treatment of myasthenia gravis / [R. Kumar, S.P. Birinder, S. Gupta et al.] // Clin. Neurol. Neurosurg. — 2015. — Vol. 19 (1). — P. 9-13. DOI: 10.4103/0972-5229.148631.

/48.jpg)