Резюме
Складна інтубація визначається як «неможливість візуалізації досвідченим анестезіологом якої-небудь ділянки голосової щілини після неодноразових спроб прямої ларингоскопії». Застосування відеоларингоскопу дозволяє отримати цінну інформацію при навчанні лікарів-інтернів, анестезіологів, лікарів медицини невідкладних станів, виявити помилки в техніці інтубації трахеї. У підсумку це дозволяє нам відпрацювати і закріпити — навчити техніці інтубації трахеї, а також поліпшити наявні навички при проведенні складної інтубації трахеї.
Трудная интубация определяется как «невозможность визуализации опытным анестезиологом какого-либо участка голосовой щели после неоднократных попыток прямой ларингоскопии». Применение видеоларингоскопа позволяет получить ценную информацию при обучении врачей-интернов, анестезиологов, врачей медицины неотложных состояний, выявить ошибки в технике интубации трахеи. В итоге это позволяет нам отработать и закрепить — научить технике интубации трахеи, а также улучшить имеющиеся навыки при проведении трудной интубации трахеи.
Difficult tracheal intubation is defined as “the inability to visualize by an experienced anesthesiologist any portion of the glottis after repeated attempts at direct laryngoscopy”. The incidence of difficult laryngoscopy reaches 8 % (Crosby et al., 1998). The incidence of difficult intubation in general is 1 : 100 intubations, failed intubation — 1 : 2,000 (Barnard O. et al., 2000). In the structure of anesthetic mortality, mortality associated with difficult intubation reaches 30 % (Miller R.D., 2007), and the incidence of “impossibility of any intubation or ventilation” ranges from 0.01 to 2 cases per 10,000 intubations (Bellhouse S.P. et al., 1996; Linkins K. et al., 2003). In the United States, there are annually registered up to 1 million of tracheal intubation conditions in emergency situations, both in and outside the hospital. About 95 % of intubations are successfully performed by anesthesiologists and emergency physicians, while the paramedics carry out a successful tracheal intubation only in 45 % of cases, indicating different levels of skills. According to Wang et al. (2011), Hubble et al. (2010), the number of successful tracheal intubation depends on the clinical experience, and is being improved with it. The authors found that in order to achieve successful intubation skills, it is necessary to perform not less than 20 difficult intubations. It is also necessary to improve the material and technical base in order to conduct difficult intubation manipulation by both young professionals, and experienced anesthesiologists and physicians of other specialties. The most common cause of a failed intubation is the inability to visualize the vocal cords. Videolaryngoscopy is a method that helps to improve the quality of understanding and perception and, consequently, to increase the “respiratory education” of doctors. Distinctive feature of videolaryngoscopy is that the visualization of anatomical structures takes place through the screen, like broncho- and endoscopes. According to Griesdale (2012), videolaryngoscopy by 80 % improves the view of the larynx as compared to direct laryngoscopy. Videolaryngoscopy have a large screen that allows you to visualize the structure of the respiratory system in real time more easily and quickly. This feature also allows the teacher to monitor and demonstrate the correctness of the tracheal intubation. Videolaryngoscopy allows you to visualize anatomical structures: the vocal cords, glottis in situations when by means of direct laryngoscopy it is impossible or difficult that reduces the risk of failed tracheal intubation. At the same time, data on the use of videolaryngoscopy in clinical practice are insufficient. Despite the published reviews and accumulated experience, techniques and indications for the use of these devices are covered incompletely. Our experience of using videolaryngoscopy is more than 6 years, both in the everyday practice of anesthesiologist, and the training of doctors — interns and students, and it allowed to identify the characteristic features of tracheal intubation. First of all, it concerns the technique of laryngoscopy during intubation. Unlike conventional laryngoscopy, when laryngoscopic blade is inserted into the right corner of the mouth and is held up to right palatine arches, blade of videolaryngoscope is put from the midline. The mistake is too deep introduction of the blade and the associated difficulty in visualizing the glottis. For a correct and quick visualization of the glottis and epiglottis, the introduction of the blade should be careful and step by step, at an average language line, repeating its anatomical shape with a constant image control. Glottis from the entrance of the esophagus should be differentiated, focusing on the following topographical landmarks: the epiglottis, vocal cords, corniculate and cuneiform tubercles. In this regard, according to recent recommendations and studies, tracheal intubation involves 4 steps (30 seconds for all stages): stage 1 — zero time — the blade is introduced into the oral cavity; stage 2 — visualization of the epiglottis and vocal cords; stage 3 — the best visualization of the entrance into the trachea; stage 4 — the introduction of the endotracheal tube into the trachea. Thus, the use of videolaryngoscopy provides valuable information not only at the time of intubation attempts, but also when training doctor interns, anesthetists, emergency physicians, enables to identify errors in the technique of tracheal intubation. As a result, it allows us to work and secure — to teach the technique of tracheal intubation, and to improve existing skills during a difficult intubation. Introduction of videolaryngoscopy in anesthetic practice is a real help for the standard fibreoptic laryngoscopy and in orotracheal intubation, including complex tracheal intubation. Mastering videolaryngoscopy is easier, as videolaryngoscope structure allows the best visualization of the laryngeal structures, and understanding intubation technique by interns reduces the risk of a failed intubation. Teaching emergency physicians the technique of tracheal intubation, both by direct laryngoscopy and videolaryngoscopy method, can improve the quality of emergency medical care for patients in critical situations and transport stages, providing clear airway, oxygenation and ventilation.
Трудная интубация трахеи определяется как «невозможность визуализации опытным анестезиологом какого-либо участка голосовой щели после неоднократных попыток прямой ларингоскопии». Частота трудной ларингоскопии достигает 8 % (Crosby et al., 1998). Частота трудной интубации в целом составляет 1 : 100 интубаций, неудавшейся интубации — 1 : 2000 (Barnard О. et al., 2000). В структуре анестезиологической летальности смертность, связанная с трудной интубацией трахеи, составляет 30 % (Miller R.D., 2007), а частота случаев «невозможности ни интубации, ни вентиляции» колеблется от 0,01 до 2 случаев на 10 тысяч интубаций (Bellhouse С.Р. et al., 1996; Linkins К. et al., 2003). В США ежегодно проводится до 1 миллиона интубаций трахеи в условиях неотложных ситуаций как в лечебных учреждениях, так и вне их. Около 95 % случаев успешной интубации проводят врачи-анестезиологи и реаниматологи, в то время как парамедикам провести успешную интубацию трахеи удается лишь в 45 % случаев, что свидетельствует о различном уровне навыков. Согласно исследованиям Wang et al. (2011), Hubble et al. (2010), количество успешных интубаций трахеи зависит от клинического опыта интубирующего и улучшается с таковым. Авторами установлено, что для достижения навыка успешной интубации трахеи необходимо провести не менее 20 трудных интубаций. Также необходимо усовершенствование материально-технической базы для освоения манипуляции «трудной интубации трахеи» как молодыми специалистами, так и опытными анестезиологами, а также врачами других специальностей.
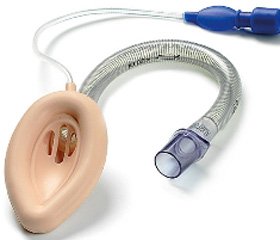
Каждый год в клинической практике врача-анестезиолога появляются новые методики интубации трахеи, в первую очередь связанные с развитием видео- и эндоскопической техники. Сегодня имеется достаточно большой арсенал устройств от фиброоптико-ларингоскопов (Airtraq, Pentax, AWS и др.) и различного типа видеоларингоскопов-модификаторов клинка Макинтоша (С-Max, GlideScope, McGrath и др.) [10], в том числе со специальными клинками для сложной интубации, до жестких ретромолярных эндоскопов-стилетов (Bonfi ls, Shikani) и фиброоптической техники [8–10]. Их особенностями в отличие от классической интубации трахеи с помощью клинков типа Макинтош и Меджил являются отличный обзор, полный визуальный контроль структур гортани и проведения интубационной трубки за голосовые связки, меньшее давление на структуры ротоглотки [2, 4, 6, 9, 11] и, как следствие, меньший стрессорный ответ и травматичность выполнения [1–3, 12]. Использование данных методов при сложной интубации трахеи внесено в протокол общества «трудные дыхательные пути» как альтернативные. Однако их применение сопряжено с целым рядом трудностей, в том числе с изменением техники ларингоскопии и интубации, необходимостью освоения эндоскопических навыков.
Наиболее частой причиной неуспешной интубации является невозможность визуализировать голосовые связки. Видеоларингоскопия является методом, который помогает улучшить качество понимания, а также восприятия и, как следствие, улучшить «дыхательное образование» у врачей. Отличительной особенностью видеоларингоскопов является то, что визуализация анатомических структур происходит посредством экрана, подобно бронхо- и эндоскопам. Согласно Бриздейлу (2012), видеоларингоскопия на 80 % улучшает обзор гортани по сравнению с прямой ларингоскопией. Видеоларингоскопы обладают большим экраном, что позволяет более просто и быстро визуализировать дыхательные структуры в реальном времени. Эта особенность также позволяет преподавателю контролировать и показывать правильность проведения интубации трахеи. Видеоларингоскопия способна визуализировать анатомические структуры: голосовые связки, голосовую щель в тех ситуациях, когда при прямой ларингоскопии это невозможно или затруднительно, что снижает риск неудачной попытки интубации трахеи.
В то же время данных об использовании видеоларингоскопии в клинической практике недостаточно. Несмотря на опубликованные обзоры [1–4, 7, 8] и накопившийся опыт, техника и показания к применению данных устройств освещены неполно.
Выделяют три интегральные причины трудной ларингоскопии и интубации трахеи (Finucane B., Santora A., 2003):
1. Ограниченный доступ к рото- или носоглотке (любое заболевание или состояние, которое ограничивает доступ ларингоскопа в рото- или носоглотку и может помешать интубации).
2. Плохая визуализация гортани (невозможность визуализации голосовой щели после введения ларингоскопа в ротоглотку и отведения мягких тканей).
3. Уменьшенная область гортани и трахеи (иногда даже при отсутствии проблем с открыванием рта или с обзором гортани трубку в гортань продвинуть невозможно).
Для прогноза риска трудной интубации трахеи важно провести клиническую оценку дыхательных путей (Millz А., 2011):
— подвижность шеи минимум на 90°;
— любой статус по Маллампати, отличный от «1»;
— наличие выступающих передних резцов;
— масса тела более 100 кг;
— трудная интубация в анамнезе.
В акушерской практике к ним добавляют (Mc Keen D.M. et al., 2011; Mills A. et al., 2010):
— возраст более 35 лет;
— отсутствие признаков родовой деятельности;
— признаки или факторы риска отека гортани (тяжелая преэклампсия или инфекции верхних дыхательных путей).
С наличием каждого из указанных факторов вероятность трудной интубации трахеи возрастает от 0 до 17 % (Elerhart L.H., 2010).
Наш опыт использования видеоларингоскопа более 6 лет как в повседневной практике врача-анестезиолога, так и в обучении врачей-интернов и курсантов позволил выделить характерные особенности при оротрахеальной интубации. В первую очередь это касается техники ларингоскопии интубации трахеи. В отличие от обычной ларингоскопии, когда клинок ларингоскопа вводится в правый угол рта и проводится до правых небных дужек, клинок видеоларингоскопа проводится сразу по средней линии [7]. Ошибкой является слишком глубокое введение клинка и связанное с этим затруднение визуализации голосовой щели. Для правильной и быстрой визуализации голосовой щели и надгортанника необходимо тщательное и пошаговое введение клинка по средней линии языка, повторяя его анатомическую форму, с постоянным контролем изображения. Голосовую щель от входа в пищевод следует дифференцировать, ориентируясь на следующие топографические ориентиры: надгортанник, голосовые связки, рожковидный и клиновидный бугорки.
В связи с этим, согласно последним рекомендациям и исследованиям, интубация трахеи включает в себя четыре этапа (30 секунд на все этапы):
— 1-й этап (время «зеро») — клинок вводится в ротовую полость;
— 2-й этап — визуализация надгортанника и голосовых связок;
— 3-й этап — наилучшая визуализация входа в трахею;
— 4-й этап — введение эндотрахеальной трубки в трахею.
Нами проведено обучение более 160 врачей-интернов и врачей медицины неотложных состояний, анестезиологов, детских анестезиологов технике интубации трахеи как методом прямой ларингоскопии, так и с помощью видеоларингоскопа. Это позволило улучшить оказание неотложной медицинской помощи врачами в критических ситуациях, на месте происшествия и этапах транспортировки пациентов в лечебные учреждения с качественным обеспечением проходимости дыхательных путей и обеспечением адекватной оксигенации и искусственной вентиляции.
M.F. Aziz et al. (2012), проведя анализ эффективности использования видеоларингоскопии в трудных ситуациях, пролили свет на все шаги в обучении и доказали преимущества ее на практике [1–6, 7, 9]. Однако видеоларингоскопия требует постоянной практики и выработки навыка обратной связи.
Поддержание квалификации включает в себя владение всеми доступными техническими и нетехническими методиками интубации трахеи, что требует постоянной практики [6, 7, 11, 12]. Применение видеоларингоскопа в обучении позволяет достичь согласованности в движениях с оценкой дыхательных путей при проведении манипуляции.
Выводы
1. Таким образом, применение видеоларингоскопа позволяет получить ценную информацию не только во время попытки интубации, но и при обучении врачей-интернов, анестезиологов, врачей медицины неотложных состояний, выявить ошибки в технике интубации трахеи. В итоге это позволяет нам отработать и закрепить — научить технике интубации трахеи, а также улучшить имеющиеся навыки при проведении трудной интубации трахеи.
2. Внедрение видеоларингоскопии в анестезиологическую практику является реальным подспорьем для стандартной ларингоскопии и фибробронхоскопии при оротрахеальной интубации трахеи, в том числе и при проблемной интубации трахеи.
3. Освоение видеоларингоскопии проще, так как строение видеоларингоскопа позволяет обеспечить наилучшую визуализацию структур гортани, а у врачей-интернов понимание техники интубации и снижает риск проведения неудачной интубации трахеи.
4. Обучение врачей медицины неотложных состояний технике интубации трахеи методом как прямой ларингоскопии, так и видеоларингоскопии позволяет улучшить качество неотложной медицинской помощи пациентам в критических ситуациях и на этапах транспортировки, обеспечивая адекватную проходимость дыхательных путей, оксигенацию и вентиляцию легких.
Конфликт интересов. Авторы заявляют об отсутствии какого-либо конфликта интересов при подготовке данной статьи.
Список литературы
1. Glidescope videolaryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-ana–lysis // Can. J. Anaesth. — 2012. — 59(1). — Р. 41-52.
2. Aziz M.F. et al. Comparative Effectiveness of the C-MAC Video Laringoscope versus Direct Laryngoscopy in the Settings of the Predicted Difficult Airway // Anesthesiology. — 2012. — 116(3). — Р. 629-636.
3. Cavus E., Neumann T., Doerges V. et al. First clinical evaluation of the C-MAC D-blade videolaryngoscope during routine and difficult intubation // Anesth. Analg. — 2011. — 112. — Р. 382-5.
4. Xue F.S., Liao X., Yuan Y.J. et al. Rational design of end-points to evaluate performance of the C-MAC D-Blade vide-olaryngoscope during routine and difficult intubation // Anesth. Analg. — 2011. — 113. — Р. 203.
5. Theodore Gar-Ling Wong. The bonfi ls retromolar intubation fi brescope: Advantages and practical aspects of its use // AJA-Online.com. — 2011. — 12. — Р. 40-8.
6. Bamgbade O.A., Onaolapo M.H., Zuokumor P.A. Nasotracheal intubation with the McGrath videolaryngoscope in patients with difficult airway // Eur. J. Anaesthesiol. — 2011. — 28(9). — Р. 673-4.
7. Behringer E.C., Kristensen M.S. Evidence for benefit vs novelty in new intubation equipment // Anaesthesia. — 2011. — 66(Suppl. 2). — Р. 57-64.
8. Niforopoulou P., Pantazopoulos I., Demestiha T. et al. Video-laryngoscopes in the adult airway management: a topical review of the literature // Acta Anaesthesiol. Scand. — 2010. — 54(9). — Р. 1050-61.
9. Hurford W.E. The video revolution: A new view of laryngoscopy // Respir. Care. — 2010. — 55(8). — Р. 1036-45.
10. Han X.D., Lin Z., Zhejiang Da Xue et al. Comparison of modified and conventional methods in orotracheal intubation of GlideScope videolaryngoscopе // Zhejiang Da Xue Xue Bao Yi Xue Ban. — 2010. — 39(1). — Р. 89-92.
11. McElwain J., Malik M.A., Harte B.H. et al. Comparison of the C-MAC videolaryngoscope with the Ma-cintosh, Glidescope, and Airtraq laryngoscopes in easy and difficult laryngo–scopy scenarios in manikins // Anaesthesia. — 2010. — 65. — Р. 483-9.
12. Mihai R., Blair E., Kay H. et al. A quantitative review and meta-analysis of performance of non-standard laryngoscopes and rigid fibreoptic intubation aids // Anaesthesia. — 2008. — 63. — Р. 745-60.