Международный эндокринологический журнал Том 15, №2, 2019
Вернуться к номеру
Захворюваність та поширеність злоякісних новоутворень щитоподібної залози в Україні та Київській області після аварії на Чорнобильській атомній електростанції
Авторы: Tkachenko V.I., Rimar Ya.Yu.
Shupyk National Medical Academy of Postgraduate Education, Kyiv, Ukraine
Рубрики: Эндокринология
Разделы: Справочник специалиста
Версия для печати
Актуальність. Щорічний приріст кількості вперше діагностованих випадків злоякісних новоутворень щитоподібної залози (ЗНЩЗ) відзначається як на територіях, найбільш забруднених радіойодом після аварії на Чорнобильській атомній електростанції (ЧАЕС), так і в інших регiонах. Неоднорідний характер регіонального зростання цієї патології потребує детального аналізу поширеності і захворюваності на ЗНЩЗ з урахуванням можливого впливу факторів ризику. Мета: провести аналіз динаміки захворюваності та поширеності ЗНЩЗ серед населення України та Київської області після аварії на ЧАЕС. Матеріали та методи. Проведено аналіз бюлетенів Національного канцерреєстру України, даних статистичних звітів закладів охорони здоров’я Київської області (2005–2016) та даних літератури починаючи з 1981 р., що містить актуальну інформацію з поточної теми. Статистичний аналіз показників було проведено за допомогою пакета програм Windows Office Exсel 2016 та StatSoft Statistica 10.0.1011.0. Результати. Починаючи з 1990 р. в Україні простежується різке зростання захворюваності на ЗНЩЗ порівняно з дочорнобильським періодом. З 1989 по 2004 р. збільшення захворюваності на рак щитоподібної залози в цілому по Україні серед чоловічого населення становило 90,28 %, а серед жіночого — 104,42 %; у Київськiй області — 65,6 та 156,9 % відповідно. За період 2005–2016 рр., окрім збільшення частки ЗНЩЗ в структурі всіх онкопатологій, також відбувся значний приріст захворюваності: по Україні — в 1,7 раза (+70 %, p < 0,01), по області — в 1,5 раза (+52,6 %, p < 0,01), з більш високими показниками захворюваності за цей період у Київській області. При проведенні гендерного аналізу (2005–2016) виявлене переважання ЗНЩЗ в жіночій популяції, а у віковій структурі найвищий приріст захворюваності відмічався серед чоловіків 40–44 i жінок 30–34 рокiв. Крім того, чітко простежувався неоднорідний характер регіонального розподілення захворюваності на ЗНЩЗ. Приріст поширеності за аналогічний період по Україні в цілому дорівнював 112,5 %, а по області — 98,2 %, прогностична модель свідчить про її збільшення протягом щонайменше наступних 5 років. Висновки. Щорічне невпинне зростання захворюваності та поширеності ЗНЩЗ, а також неоднорідне гендерне, вікове та регіональне розподілення досліджуваних показників свідчить про багатофакторність та актуальність вивчення цієї проблеми з подальшим покращанням системи профілактичних заходів.
Актуальность. Ежегодный прирост количества впервые диагностированных случаев злокачественных новообразований щитовидной железы (ЗНЩЖ) отмечается как на территориях, наиболее загрязненных радиойодом после аварии на Чернобыльской атомной электростанции (ЧАЭС), так и в других регионах. Неоднородный характер регионального роста данной патологии требует детального анализа распространенности и заболеваемости ЗНЩЖ с учетом возможного влияния факторов риска. Цель: провести анализ динамики заболеваемости и распространенности ЗНЩЖ среди населения Украины и Киевской области после аварии на ЧАЭС. Материалы и методы. Проведен анализ бюллетеней Национального канцерреестра Украины, данных статистических отчетов учреждений здравоохранения Киевской области (2005–2016) и данных литературы начиная с 1981 г., которая содержит актуальную информацию по текущей теме. Статистический анализ показателей выполнен с помощью пакета программ Windows Office Exсel 2016 и StatSoft Statistica 10.0.1011.0. Результаты. Начиная с 1990 г. в Украине прослеживается резкий рост заболеваемости ЗНЩЖ по сравнению с дочернобыльским периодом. С 1989 по 2004 г. увеличение заболеваемости раком щитовидной железы в целом по Украине среди мужского населения составило 90,28 %, а среди женского — 104,42 %; в Киевской области — 65,6 и 156,9 % соответственно. За период 2005–2016 гг., помимо увеличения доли ЗНЩЖ в структуре всех онкопатологий, также отмечен значительный прирост заболеваемости: по Украине — в 1,7 раза (+70 %, p < 0,01), по области — в 1,5 раза (+52,6 %, p < 0,01), с более высокими показателями заболеваемости за данный период в Киевской области. При проведении гендерного анализа (2005–2016) обнаружено преобладание ЗНЩЖ в женской популяции, а в возрастной структуре самый высокий прирост заболеваемости отмечался среди мужчин 40–44 и женщин 30–34 лет. Кроме того, четко прослеживался неоднородный характер регионального распределения заболеваемости ЗНЩЖ. Увеличение распространенности за аналогичный период по Украине в целом составило 112,5 %, а по области — 98,2 %, прогностическая модель свидетельствует о ее повышении в течение по меньшей мере следующих 5 лет. Выводы. Ежегодный постоянный рост заболеваемости и распространенности ЗНЩЖ, а также неоднородное гендерное, возрастное и региональное распределение исследуемых показателей свидетельствует о многофакторности и актуальности изучения данной проблемы с последующим улучшением системы профилактических мероприятий.
Background. The annual increase in the number of newly diagnosed cases of malignant neoplasms of the thyroid gland (MNTG) is observed both in the territories most contaminated with radioiodine after the Chernobyl accident, and in other regions. The heterogeneous nature of the regional increase of this pathology requires a detailed analysis of the prevalence and the morbidity rate of MNTG, taking into account the possible influence of risk factors. The purpose was to analyze the morbidity rate and the prevalence of MNTG among the population of Ukraine and Kyiv region after the Chernobyl Nuclear Power Plant accident. Materials and methods. The analysis of the bulletins of the National Cancer Registry of Ukraine, the data of statistical reports of healthcare institutions of Kyiv region (2005–2016) and literature data since 1981, which contained relevant information on the subject was performed. Statistical analysis of indicators was carried out using software package Windows Office Excel 2016 and StatSoft Statistica 10.0.1011.0. Results. Since 1990 in Ukraine, there has been a sharp increase in the morbidity rate of MNTG compared with the pre-Chernobyl period. From 1989 to 2004, the all-Ukrainian rate of increase in the morbidity rate of thyroid cancer among male population was 90.28 %, and among females — 104.42 %; for Kyiv region — 65.6 and 156.9 %, respectively. In 2005–2016, in addition to increase in the share of MNTG in the structure of all cancer pathologies, there was also a significant increase in the morbidity rate: 1.7-fold in Ukraine (+70 %, p < 0.01) and 1.5-fold in the region (+52.6 %, p < 0.01), with higher incidence rates for this period in Kyiv region. Gender analysis (2005–2016) revealed the prevalence of thyroid cancer in the female population, and in terms of the age structure, the highest rate of increase in the morbidity rate was observed among men aged 40–44 and women aged 30–34 years. In addition, the heterogeneous nature of the regional distribution of the morbidity rate was clearly observed. The rate of increase in prevalence over the same period in Ukraine as a whole was 112.5 %, and in the region — 98.2 %, the predictive model showed its increase over at least next 5 years. Conclusions. The annual steady increase in the morbidity rate and prevalence of MNTG, as well as the heterogeneous gender, age and regional distribution of the studied parameters indicates the multifactoriality and relevance of studying this problem with the subsequent improvement of the system of preventive measures.
рак щитоподібної залози; злоякісні новоутворення щитоподібної залози; епідеміологія; захворюваність; поширеність; фактори ризику; Україна; Київська область
рак щитовидной железы; злокачественные новообразования щитовидной железы; эпидемиология; заболеваемость; распространенность; факторы риска; Украина; Киевская область
thyroid cancer; malignant neoplasms of the thyroid gland; epidemiology; morbidity rate; prevalence; risk factors; Ukraine; Kyiv region
Introduction
In recent decades, cancer has a tendency to increase both in the world and in Ukraine. The International Agency for Research on Cancer predicted 567,233 new cases of thyroid cancer (TC) in the world in 2018, representing 3.1 % of all cancer cases [1].
In Ukraine, the ratio of malignant neoplasms of the thyroid gland (MNTG) in the structure of cancer morbidity for 15 years has increased from 1.3 % in 2002 to 2.3 % in 2016, that is, by 1.8 times. As of 2016, MNTG rank fourth in the gender–age structure of malignant neoplasms among the Ukrainian female population aged 0–17 and 30–54 years, and among women aged 18–29 years, it ranks first [2].
High prevalence of TC in Ukraine is associated primarily with carcinogenic effect of ionizing radiation due to the Chernobyl accident, which led to a sharp increase in the number of radiation–induced tumors of the thyroid gland, starting from 4–5 years after the accident, and continuing its effect till now. It is reliably known that people who were 0–18 and especially 0–5 years old at the time of the accident, were most exposed to ioni–zing radiation [3, 4]. However, the number of newly diagnosed cases of TC annually increases not only in the most radioactive contaminated territories, but also in other regions. Thus, according to the latest information of 2017, the morbidity rates of MNTG were highest in Kirovohrad (14.6 0/0000), Vinnytsia (13.6 0/0000), Sumy (12.8 0/0000), Kyiv (12.1 0/0000) regions and in Kyiv (12.7 0/0000), whereas the lowest indicators were observed in Transcarpathi–an (1.8 0/0000), Chernivtsi (3.1 0/0000), Volyn (3.8 0/0000), Odesa (4.2 0/0000) and Ivano– Frankivsk (4.4 0/0000) regions [2]. This heterogeneous regional distribution indicates the possible influence of anthropogenic factor, micronu–trient deficiency, concomitant diseases of the thyroid gland and various organs and systems, as well as a number of other risk factors that can provoke neoplastic process or directly modify carcinogenesis [5–9]. Referring to the above–mentioned and due to the disabling effects of this pathology, the analysis of the morbidity rate and the prevalence of MNTG in the regions of Ukraine ta–king into account possible risk factors is of current inte–rest, as it will contribute to the development of measures for improving MNTG treatment in Ukraine.
The purpose: to analyze the morbidity rate and the prevalence of MNTG among the population of Ukraine and Kyiv region after the Chernobyl Nuclear Power Plant accident.
Materials and methods
To evaluate the morbidity rate and the prevalence of MNTG, there were used bulletins of the National Cancer Registry of Ukraine, data from statistic reports of the healthcare institutions of Kyiv region (2005–2016) and literature data since 1981, which contained relevant information on the subject.
Statistical analysis of indicators was carried out using software package Windows Office Exсel 2016 and StatSoft Statistica 10.0.1011.0.
Results
The data of the retrospective analysis showed that in the pre–Chernobyl period, the morbidity of MNTG was episodic; the diagnostic capabilities, as well as the access to statistical indicators were limited at that time, but observation of A.D. Chernobrovyi (2001) shows rather low morbidity rate of TC among Ukrainian population before the Chernobyl accident. Thus, in 1981–1985, the morbidity of TC averaged 0.62 0/0000, and from 1986 to 1999, there was the clear annual increase in the morbidity rate of TC in Ukraine — up to 4.0 0/0000, it was especially intensive since 1990, in particular among the population of Kyiv, Chernihiv and Zhytomyr regions, as well as in Kyiv residents [10, 11]. This is due to the start of the minimum latent period for the development of radiation–induced TC in a group of people who were 0–18 years old at the time of the accident, which is likely to continue until now [3, 12].
In addition, the research findings of M.M. Fuzik et al. over the period of 1989–2010 showed a significantly higher increase in the level of TC morbidity and its ave–rage annual rate in regions with high radiation exposure (> 35 mGy) compared to all other regions of Ukraine (≤ 35 mGy), both among those who were children and adolescents at the time of the Chernobyl accident and adult population [13].
Accurate record of statistical indicators on MNTG morbidity in Ukraine has been started in 1989 with the help of the program information system of cancer re–gistration by the National Cancer Institute when the Decree of the Ministry of Health of Ukraine No. 10 “About the creation of the National Cancer Registry of Ukraine” dated January 2, 1996 was approved [14]. According to the epidemiological research by V.M. Horbenko et al. over the period of 1989–2004, the morbidity rate of TC in Ukraine among male population increased from 1.01 to 1.92 0/0000, and among women — from 3.54 to 7.24 0/0000, i.e., 90.28 and 104.42 %, respectively. The rate of increase in the morbidity rate in Kyiv region among male population was lower (65.6 %) than in other regions of the country, but among women it accounted for 156.9 % that was higher than the corresponding figu–res in Ukraine [15]. Regional analysis of the morbi–dity rate of TC in 1989–2004 showed that the highest increase among men was observed in Zhytomyr, Ivano–Frankivsk, Sumy and Zaporizhzhia regions, as well as in Kyiv; among women — in Cherkasy, Sumy, Zhytomyr, Poltava and Zaporizhzhia regions. Therefore, the researchers noted that an increase in the morbidity rate of TC in Ukraine is the highest among malignant neoplasms of other localization [15].
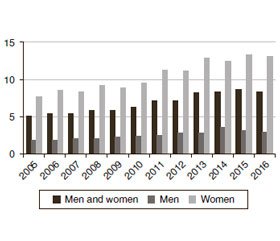
To continue studying the morbidity rate and the prevalence of MNTG in Ukrainian population as a whole and in Kyiv region in particular, we have analyzed statistical data for 2005–2016. It was found that in the structure of all cancers, the share of MNTG in Ukraine increased from 1.4 to 2.3 % (rate of increase +64.3 %), in Kyiv region — from 2.6 to 3.6 % (rate of increase +38.5 %). The morbidity rate of MNTG in Ukraine increased by 1.7 times — from 5 to 8.5 0/0000 (rate of increase +70 %, p < 0.01), in Kyiv region — by 1.5 times, from 9.5 to 14.5 0/0000 (rate of increase +52.6 %, p < 0.01) (Fig. 1).
However, along with morbidity rate of MNTG, which was higher in Ukraine than in Kyiv region, the mean morbidity rate in region (12.8 0/0000) was determined as more significant comparing to the nationwide (6.9 0/0000). In addition, the morbidity rates of MNTG among the population of Kyiv region for 2005–2016 were always statistically higher (p < 0.01) than the indicators in Ukraine, in the presence of certain fluctuations.
Heterogeneous nature of the fluctuations in the morbidity rate of MNTG in Kyiv region needs further in–depth study. It can be assumed that one of the additional factors is the variable concentration of carcinogenic substances in the air. Thus, S.M. Tsymbaliuk et al. (2017) established a strong correlation (p < 0.05) between the levels of air pollution by chemical carcinogens, namely chromium IV, benzo[a]pyrene, formaldehyde and cadmium, in Kyiv and Cherkasy and the prevalence of TC. The authors also proved that the time lag of the grea–test manifestation of the cumulative phenomenon for development of TC is 10 years [17]. The influence of anthropogenic chemical factors on the development of TC was also studied by N.V. Balenko et al. [8, 17]. The authors concluded that some compounds, in particular pesticides of different chemical structures, perchlorates, and the socio–economic characteristics of the regions of Ukraine, determine the morbidity rate of TC, and the question of studying the ways and consequences of their effects remains unsettled until today [8, 17].
Moreover, a comparative analysis of the morbidity rate of MNTG in the regions of Ukraine over the re–levant years has shown the highest increase among men in Vinnytsia, Khmelnytskyi, Volyn, Sumy and Zapori–zhzhia regions (Table 1). An increase in the morbi–dity rate among men in Vinnytsia region was surprisingly high — 1,325 % (from 0.4 to 5.7 0/0000). The most significant increase in the morbidity rate among women was in Volyn, Kirovohrad, Ternopil, Khmelnytskyi and Sumy regions. In Volyn region, the morbidity rate among women in 2005–2016 has increased from 1.1 to 7.3 0/0000 (rate of increase 563.6 %).
To provide a more detailed analysis of the dynamics of morbidity rate of MNTG, we divided the period from 1999 to 2013 into 5–year intervals: 1999–2003, 2004–2008, 2009–2013; since 2014, there are no data from Luhansk and Donetsk regions, Sevastopil and the Autonomous Republic of Crimea. It was found that the increase in the morbidity rate in Ukraine for the first period was 7.1 %, for the second — 22.9 %, for the third — 40.7 %, while in Kyiv region it was 9.4, 44.7 and 19.7 %, respectively.
The findings indicate that the rate of increase in the morbidity in Kyiv region was higher than in Ukraine du–ring the first two periods (1999–2003 and 2004–2008), and it slows down in 2009–2013 that can be explained by a decrease in the stochastic effect of radiation pollution in the studied territory after the Chernobyl accident. On the other hand, according to the findings of S.M. Tsymbaliuk et al. [18], an increase in standardized indicators of the morbidity rate of MNTG (the Ukrainian standard) for 1991–2013 in the areas with high radiation control, which include Kyiv, Zhytomyr, Rivne, Volyn and Chernihiv regions, averaged 2.58 ± 0.14 times and was lower than in regions with high industrial development and in predominantly agricultural areas. It proves the possible influence of other carcinogens, in particular those of anthropogenic origin, except for the well–known influence of ionizing radiation, and combined effects of iodine deficiency of varying severity, which is observed in many regions of Ukraine, including Kyiv region, that must be taken into consideration [4, 5].
Discussion
Today, according to many national and foreign stu–dies, it is known that the development of MNTG depends on gender. It has been found that women have TC on average 3–5 times more often than men [19]. Gender analysis of statistical indicators of the morbidity rate of MNTG among female population in 2005–2016 showed 1.7–fold increase, both in Ukraine as a whole (from 7.8 to 13.2 0/0000; rate of increase +69.2 %, p < 0.01), and in Kyiv region (from 14.1 to 23.6 0/0000; rate of increase +67.4 %, p < 0.01). The national index of morbidity among male population increased by 1.6 times (from 1.9 to 3.0 0/0000, rate of increase +57.9 %, p < 0.01), while in Kyiv region, there were observed heterogeneous fluctuations of indicators, but the average annual rate of morbidity increase among men (3.3 %) indicated a trend towards moderate growth. The men to women ratio in the total number of patients with MNTG in Ukraine in 2016 was 1 : 5, and in the region — 1 : 7. Over the whole analyzed period, the morbidity rate of MNTG among female population in Kyiv region was 2.7–6.3 times higher, and in Ukraine — 3.5–4.5 times higher than among men. This type of gender heterogeneity clearly shows the importance of certain hormonal factors, such as the age of menarche and menopause, the age of the first labor and their number, as well as the presence of some gynecological diseases, the effect of which has been actively studied recently [19–21].
Describing the age structure of the first diagnosed cases of MNTG in Ukraine for 2005–2016, we can distinguish a certain “rejuvenation” of the period with hig–hest rates of morbidity, especially among women (Fig. 2). For exam–ple, if in 2005 the morbidity rate was maximal among women aged 55–59 years and men aged 80–84, then in 2016, a significant increase begins with the age of 30–34, and the maximum values correspond to 55–59 years in the structure of both genders. When assessing the rate of increase in the morbidity rate of MNTG, this trend was also observed in the form of the highest percentage values for the following age intervals: 40–44 years among men and 30–34 years among women. In addition, from the age of 80 years and over, the morbidity was characterized by a decline both among male and female population, which may indicate a need for more careful monitoring of thyroid neoplasms in young people.
When analyzing the prevalence of the studied oncologic pathology from 2005 to 2016, a similar epidemiological situation was observed: regional indicators for each year almost twice exceeded the corresponding national figures and were statistically higher (p < 0.01). An increase in the prevalence of MNTG for this period in Kyiv region among the overall population was 98.2 % (from 114.3 to 226.5 0/0000; p < 0.01), and in Ukraine it was 112.5 % (from 50.2 to 106.7 0/0000; p < 0.01).
Using the trend line to further evaluate the epidemiological situation, we predicted the prevalence of TC in 2017–2021 in Kyiv region and in Ukraine (Fig. 3). In the prognostic calculation of the dynamics of the TC prevalence for 5 years, the regression analysis demonstrated a polynomial (2–level) long–term trend line with high determinants (R2). Thus, in Kyiv region, the calculated R2 accounted for 0.9851 and was close to 1, which demonstrates the high accuracy of the selected regression equation and the adequacy of the model. The polynomial trend of the TC prevalence in Ukraine was also characterized by a significant R2 index (0.9791), which, in turn, shows that the chosen prediction model (97.9 %) indicates an adequate selection of the trend equation to the initial data. Thus, the prognosis of the TС prevalence shows its growth over the next 5 years, both in Kyiv region and in Ukraine, which clearly demonstrates the need to improve primary and secondary prevention at different levels of health care provision.
Conclusions
The retrospective analysis of statistical data showed that after the Chernobyl accident, the morbidity rates of MNTG were characterized by constant growth since 1986, with greater intensity after 1990, with the onset of the ionizing radiation effects, especially in the most affected regions.
Over the period of 2005–2016, the morbidity rates of MNTG increased in Ukraine and in Kyiv region by 1.7 and 1.5 times, and in Kyiv region, the rates were statistically significantly higher than in Ukraine (p < 0.01) and were characterized by certain fluctuations. The revealed heterogeneous rates of increase in the morbidity of MNTG in various age groups and the highest morbi–dity among young people also indicate the influence of age factors on oncogenesis and “rejuvenation” of MNTG. A significant increase (3–6–fold) in the morbidity rate of MNTG among female population as compared to male population during all the time both in Kyiv region and in Ukraine indicates the contribution of certain gender factors. The highest rate of increase in the morbidity rate of MNTG among male population was observed in Vinnytsia (1,325 %), Khmelnytskyi (266.7 %), Volyn (233.3 %), Sumy (104.8 %), and Zaporizhzhia (87.5 %) regions, and among women — in Volyn (563.6 %), Kirovohrad (242.7 %), Ternopil (189.3 %), Khmelnytskyi (152.2 %) and Sumy (151.3 %) regions, indicating not only carcinogenic and stochastic effect of ionizing radiation, but also the influence of other factors.
The prevalence of TC in 2005–2016 has the follo–wing rates of increase: in the region — 98.2 % (p < 0.01), in Ukraine — 112.5 % (p < 0.01), and further increase is expected.
The obtained results indicate the multifactoriality and urgency of the problem that requires further systema–tic study, as well as demonstrate the need for a directed system of preventive measures to improve the cancer situation in Ukraine.
Conflicts of interests. Authors declare no conflicts of interests that might be construed to influence the results or interpretation of their manuscript.

/154-1.jpg)
/154-2.jpg)
/155-1.jpg)
/155-2.jpg)