Международный эндокринологический журнал Том 16, №6, 2020
Вернуться к номеру
Thyrotoxic Periodic Paralysis: A Rare Case
Авторы: Deniz İncaman(1), Musa Salmanoğlu(2), Ömür Tabak(3), Abdulbaki Kumbasar(3)
(1) — Kastamonu Training and Education Hospital, İnternal Medicine Clinic, Kastamonu, Turkey
(2) — Health Science University, Sultan Abdulhamid Han Training and Education Hospital, İstanbul, Turkey
(3) — Health Science University, İstanbul Kanuni Sultan Süleyman Training and Education Hospital, İnternal Medicine Clinic, İstanbul, Turkey
Рубрики: Эндокринология
Разделы: Справочник специалиста
Версия для печати
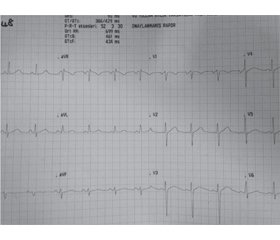
Тиреотоксичний гіпокаліємічний періодичний параліч є рідкісним спадковим захворюванням, що характеризується періодичною втратою сили м’язів. У проведеному дослідженні діагностовано періодичний гіпокаліємічний параліч у результаті обстеження пацієнта у відділенні невідкладної допомоги. Оскільки цей випадок рідкісний, література подана з оглядом. 43-річний пацієнт чоловічої статі з відомою грижею поперекового диска в анамнезі був доставлений до екстреної служби лікарні зі скаргою на неможливість рухати тілом, коли прокинувся о 6:00 ранку. Пацієнт приймав метимазол у таблетках 12 годин тому через скарги на головний біль. Вечеря складалася з продуктів з високим вмістом вуглеводів. Клінічний огляд виявив артеріальний тиск 105/70 мм рт.ст., частоту серцевих скорочень 93 на 1 хв, температуру 36,8 градуса, загальну втрату сили в чотирьох кінцівках та тетраплегію. Втрати чутливості, офтальмопатії, тремору не виявлено, ізохоричний та світловий рефлекс зіниць був двобічним, рефлекс ахіллова сухожилля прийнятий за гіпоактивний. Розміри очей були нормальними, щитоподібна залоза не збільшена. Цей випадок оцінювали як тиреотоксичний періодичний параліч, враховуючи час початку нападів, зокрема після вечері з високим вмістом вуглеводів, що спричиняє параліч, поліпшення симптомів при проведенні замісної терапії, вміст калію в сироватці крові, тести функції щитоподібної залози та результати електрокардіограми. У підсумку тиреотоксичний періодичний параліч слід розглядати як диференціальний діагноз у молодих, особливо в пацієнтів чоловічої статі, які страждають від рухового паралічу. Визначення гормонів щитоподібної залози та рівня калію допомагає в діагностиці.
Тиреотоксический гипокалиемический периодический паралич является редким наследственным заболеванием, характеризующимся периодической потерей силы мышц. В проведенном исследовании диагностирован периодический гипокалиемический паралич в результате обследования пациента в отделении неотложной помощи. Поскольку этот случай редкий, представлен обзор литературы. 43-летний пациент мужского пола с известной грыжей поясничного диска в анамнезе был доставлен в экстренную службу больницы с жалобой на невозможность движения телом после пробуждения в 6:00 утра. Пациент принимал метимазол в таблетках 12 часов назад из-за жалоб на головную боль. Ужин состоял из продуктов с высоким содержанием углеводов. Клинический осмотр выявил артериальное давление 105/70 мм рт.ст., частоту сердечных сокращений 93 в 1 мин, температуру 36,8 градуса, общую потерю силы в четырех конечностях и тетраплегию. Потери чувствительности, офтальмопатии, тремора не обнаружено, изохорический и световой рефлекс зрачков двусторонний, рефлекс ахиллова сухожилия принят за гипоактивный. Размеры глаз нормальные, щитовидная железа не увеличена. Этот случай оценивали как тиреотоксический периодический паралич, учитывая время начала приступов, особенно после ужина с высоким содержанием углеводов, вызывающим паралич, улучшение симптомов при проведении заместительной терапии, содержание калия в сыворотке крови, тесты функции щитовидной железы и результаты электрокардиограммы. В итоге тиреотоксический периодический паралич следует рассматривать как дифференциальный диагноз у молодых, особенно у пациентов мужского пола, страдающих от двигательного паралича. Определение гормонов щитовидной железы и уровня калия помогает в диагностике.
Hypokalemic periodic paralysis is a rare hereditary disease characterized by recurrent muscle strength loss.It is a reversibl disease that is clinical presentation with tiredness and paralysis that develops over hours and days.There are precipitative factors such as stress, exercise, carbohydrate-rich nutrition that trigger the formation of episodes. In our study, hypokalemic periodic paralysis was diagnosed as a result of a tetraplegic examination of a patient in our emergency department. Because this case is rare, the literature has been presented with review. A 43-year-old male patient with a known history of lumbar disc hernia was brought to the emergency service of our hospital with the complaint of being unable to move his body when he woke up at 06:00 in the morning. He used 1 oral metamizole sodium 12 hours ago due to headache complaint, and he was fed with high carbohydrate content at dinner. Physical examination revealed a blood pressure of 105/70 mm/hg, a pulse of 93/min, a temperature of 36.8 degrees, a total loss of strength in four extremities, and tetraplegia. Sensory loss, ophthalmopathy, tremor were not detected, pupillary isochoric and light reflex was bilateral, achilles tendon reflex was taken as hypoactive. Eye sizes were normal, thyroid tissue was non-palpable. This case was evaluated as TPP because of the time of onset of attacks, the onset after high-carbohydrate feeding, causing paralysis, improvement of symptoms with replacement, serum potassium, thyroid function tests, and ECG findings. His dramatic response to treatment supported our recognition. In conclusion, it should be considered as a differential diagnosis in young and especially male patients presenting with TPP motor paralysis, which is rare. Determination of thyroid hormones and potassium levels helps in diagnosis.
тиреотоксикоз; тиреотоксичний періодичний параліч; гіпокаліємія
тиреотоксикоз; тиреотоксический периодический паралич; гипокалиемия
thyrotoxicosis; hypokalemic periodic paralysis; hypokalaemia
Introduction
Clinical case
Discussion
Conclusions
- Lin S.H. Thyrotoxic periodic paralysis. Mayo Clin. Proc. 2005. 80(1). 99-105. doi: 10.1016/S0025-6196(11)62965-0.
- Fontaine B., Lapie P., Plassart E., Tabti N., Nicole S., Reboul J., Rime-Davoine C.S. Periodic paralysis and voltage-gated ion channels. Kidney Int. 1996. 49(1). 9-18. doi: 10.1038/ki.1996.2.
- Manoukian M.A., Foote J.A., Crapo L.M. Clinical and metabolic features of thyrotoxic periodic paralysis in 24 episodes. Arch. Intern. Med. 1999. 159. 601-606. doi: 10.1001/archinte.159.6.601.
- Griggs R.C., Resnick J., Engel W.K. Intravenous treatment of hypokalemic periodic paralysis. Arch. Neurol. 1983. 40. 539-540. doi: 10.1001/archneur.1983.04050080039005.
- Ko G.T.C., Chow C.C., Yeung V.T.F., Chan H.H.L., Li J.K.Y., Cockram C.S. Thyrotoxic periodic paralysis in a Chinese population. QJM. 1996. 89. 463-8.
- Hakan Şıvgın, Türker Taşlıyurt, Ersegül İnce, Şafak Şahin, Süheyla Uzun Kaya, Banu Öztürk, İki Farklı Tipte. Periyodik Paralizi Olgusu: Ailesel ve Tirotoksik Periyodik Paralizi. Gaziosmanpaşa Üniversitesi Tıp Fakültesi Dergisi. 2013. 5(3). 153-158.
- Ryan D.P., da Silva M.R., Soong T.W., Fontaine B., Donaldson M.R., Kung A.W. et al. Mutations in potassium channel Kir2.6 cause susceptibility to thyrotoxic hypokalemic periodic paralysis. Cell. 2010. 140(1). 88-98. doi: 10.1016/j.cell.2009.12.024.
- Ferda Selçuk, Senem Mut. Kortikosteroid ile İndüklenen Hipokalemik Periyodik Paralizi: İki Olgu Sunumu. Ankara Üniversitesi Tıp Fakültesi Mecmuası. 2016. 69(3). 211-212. doi: 10.1501/Tipfak_0000000947.
- Kilpatrick R.E., Seiler-Smith S., Levine S.N. Thyrotoxic hypokalemic periodic paralysis: report of four cases in black American males. Thyroid. 1994. 4(4). 441-5. doi: 10.1089/thy.1994.4.441.
- Gorchynski J., Nwosu H., Frame J. Acute ascending paralysis presenting as an endocrine emergency. Am. J. Emerg. Med. 2009. 27. 371. doi: 10.1016/j.ajem.2008.07.018.
- Lam L., Nair R.J., Tingle L. Thyrotoxic periodic paralysis. Proc. (Bayl. Univ. Med. Cent.). 2006. 9(2). 126-9. doi: 10.1080/08998280.2006.11928143.
- Sthaneshwar P., Prathibha R., Yap S.F. Thyrotoxic periodic paralysis: a report of 3 Malaysian cases and a review of its pathology. Malays J. Pathol. 2005. 27(1). 29-32. PMID: 16676690.
- Manoukian M.A., Foote J.A., Crapo L.M. Clinical and metabolic features of thyrotoxic periodic paralysis in 24 episodes. Arch. Intern. Med. 1999. 159(6). 601-606. doi: 10.1001/archinte.159.6.601.

/86.jpg)