Introduction
Both sodium ions and water are the most important components of the intra and extracellular environment. Sodium ions play a pivotal role in maintaining homeostasis. In order to maintain homeostasis, serum osmolality must be kept within normal limits. Living organisms do so by kee-ping sodium ions and water concentration into a certain limit which is vital for the normal functioning of the brain and other vital organs. The addition of a large quantity of sodium or excessive loss of water badly affects the tonicity of blood. The increase of sodium ions in the blood can be acute or chronic. Acute rise of serum sodium ion concentration more than 145 mmol/L in less than 48 hours is termed acute hypernatremia. Acute hypernatremia can be due to multiple reasons, e.g., acute free water loss or high sodium intake such as infusion of hypertonic saline, ingestion of large quantities of table salt, application of sodium chloride on burn wounds etc. [1–3].
Case Report
A 59 years old female patient known case of hydatid liver disease was admitted to the intensive care unit from the ope-ration room as a case of acute hypernatremia post ruptured and infected hydatid cyst excision.
The patient was diagnosed with liver hydatid cyst 6 years ago in Morocco and underwent hydatid cyst excision there. Nearly 5 months ago, the patient complained of cough with brownish sputum. She went to a local hospital and an ultrasound examination showed multiple lesions, the biggest one in segment 8 of liver measuring 10 × 14 cm. Her CT scan revealed a hydatid cyst in middle lobe of the right lung having communication or a fistula with a liver hydatid cyst.
This patient was referred to our hospital for thoracic, hepatobiliary/interventional radiology opinion and mana-gement. She was examined by a thoracic surgeon and shif-ted the care to hepatobiliary service for further management. Four days later, the interventional radiologist was consulted for possible drainage catheter insertion into the liver hydatid cyst under ultrasound guidance. A pigtail catheter was inserted into the liver hydatid cyst cavity without any complications. The culture of the cyst fluid showed Echinococcus granulosus and the patient was put on albendazole. She was followed up by hepatobiliary service. After one month, she was discharged home with a pigtail catheter in place after almost 2 weeks of our inpatient treatment.
After 2 months, Percutaneous Aspiration Injection and Re-aspiration (PAIR) procedure was done by an interventional radiologist, and the pigtail catheter was removed. The patient continued to follow hepatobiliary service on an outpatient basis with a serial ultrasound abdomen.
2 months later, a CT scan abdomen showed an increase in size of the liver cyst with the anterior abdominal wall and subhepatic collections. The patient was admitted to the surgical floor for elective laparotomy and washing of the peritoneal cavity with hypertonic saline. Her pre- and postoperative laboratory values of interest are shown below.
During midline laparotomy, the surgical findings were as follows:
1 — Right upper abdominal wall subcutaneous and intramuscular purulent fluid collection along with hydatid cyst cavity connected to subhepatic space containing hydatid germinal membranes and daughter cysts.
2 — No intra-abdominal spread of hydatid disease.
So the following surgical procedure was done.
1 — Aspiration of hydatid fluid, daughter cysts, and pus.
2 — Removal of hydatid germinal membranes.
3 — The subcutaneous collection of pus was drained through a direct incision on it.
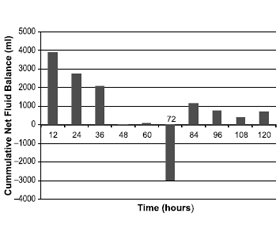
Peritoneal and hydatid cyst cavity was washed with hypertonic saline (14.6 %) for 40 to 60 minutes and then aspirated and rewashed with normal saline before abdominal wall closure. Serum sodium level was checked at that time during the procedure and it jumped to 180 mmol/l and later to 197 mmol/l just after the aspiration of hypertonic saline from the peritoneal cavity. She was having a normal serum sodium level of 143 mmol/l preoperatively. Due to the acute severe hypernatremia, the patient was immediately shifted to ICU for further management. Her laboratory serum sodium levels over time have been shown in Fig. 1. Please note that these laboratory serum sodium values have not been corrected with serum glucose levels.
Serum sodium level can be corrected according to the following formula, Corrected serum Sodium = measured sodium + [1.6 (Glucose – 100)]/100 or simply by adding 1.6 mEq/L for every 100 mg/dl increase in serum glucose.
During 2nd hour of ICU admission, the patient started to have hypotension with sinus tachycardia that did not respond to bolus IV fluids, so we started norepinephrine infusion at the rate of 0.01 microgram/kg/min and escalated to 0.5 microgram/kg/min to achieve a mean arterial pressure of around 65 to 70. We further added epinephrine infusion to treat her potential anaphylactic reaction that could have been arisen possibly due to hydatid fluid instillation into the peritoneal cavity. She was put on chlorpheniramine 10 mg I.V three times a day for 2 days, hydrocortisone 200 mg I.V stat and 100 mg I.V three times a day for 2 days, and later tapering doses till off in the following 24 hours. She remained on norepinephrine infusion for 2 hours and then discontinued but epinephrine infusion continued for the next 16 hours and then weaned off as the patient became hemodynamically stable.
The patient was kept nil per oral (NPO) and started partial parenteral nutrition (PPN) after 28 hours of ICU admission in the form of dextrose 25 % at the rate of 30 ml/h plus amino plasma at the rate of 20 ml/h.
She remained on a controlled mode of ventilation for the initial 24 hours and later weaned to assisted synchronized ventilation. She was kept at Richmond Agitation Sedation Score (RASS) of –1 to 0 with the help of fentanyl and midazolam infusions. On the 2nd post (44 hrs. after ICU admission) operative day, we assessed her neurologically after holding sedation/analgesia, she was fully conscious, oriented, and obeying commands by her all four limbs. Her suitability for extubation was assessed and extubated successfully.
Antimicrobial coverage was started empirically in the form of vancomycin 1 gram daily with the next pre-dose level and meropenem 1 gram thrice a day. Fluconazole was added as 400 mg I.V daily after 24 hours of ICU admission on an empirical basis.
After 40 hours of ICU admission, we received abdominal drain fluid culture and sensitivity result as MDR Acinetobacter baumannii while her blood, tracheal aspirate, and urine cultures were all negative. Meropenem was escalated to 2 grams thrice a day and vancomycin dose increased to 1 gram twice a day to tackle her increasing white blood cell count. Tigecycline was added as 100 mg I.V stat and 50 mg I.V twice a day as white blood cell count increased to 44,000/c after 72 hours of ICU admission.
The very next day (after 90 hours), we added colistin as 9 million international Units (I.U) IV stat and 4.5 million I.U twice a day. To treat her hydatid disease, we continued her regular dose of albendazole 400 mg twice a day.
On a post-operative day 6, we discontinued vancomycin and Fluconazole.
She was transferred to the surgical floor on the 7th post-operative day without any neurological or ICU-related complications with normal levels of serum sodium and other electrolytes.
Discussion
Acute intra-operative hypernatremia is rare but once it happens, it leads to severe neurological complications and high mortality [2]. Mortality rate can jump up to 70 % with an acute rise of serum sodium to 160 mm/l. It has been observed that adults suffer more complications than children due to acute hypernatremia. There are only a few case reports of successful recovery from acute iatrogenic hypernatremia in adults [3].
R.C. Goldszer and E.L. Coodley have reported a case of acute hypernatremia (202 mmol/l) in a 74-year old lady that recovered successfully without any neurological complication although she remained comatose for 7 days. In this case, hypernatremia happened due to excessive insensible water loss in hot weather with an inability to take adequate water [4].
P.E. Ozcan, A. Yavru et al. have reported a case of acute iatrogenic hypernatremia (185 mmol/l) during hepatic hydatid cyst removal in a 55-year-old lady. The patient was extubated post-operatively but re-intubated immediately due to decreased level of consciousness. Her serum sodium level was found to be 185 mmol/l and hence transferred to ICU for further monitoring. She became conscious and was successfully extubated after 36 hours of ICU stay [5].
J.L. Dobato, F.J. Barriga et al. have reported a case of iatrogenic hypernatremia (176 mmol/l) in a 37 years old man. This patient had liver hydatid cyst ruptured into the peritoneal cavity that was treated with peritoneal lavage with hypertonic saline but the patient developed extra pontine myelinolysis followed by a syndrome of isolated amnesia due to bilateral hippocampal lesions [6].
Echinococcus granulosis — a tapeworm, is the causative agent of hydatid disease. Humans are among the intermediate hosts. In humans, this parasite produces cysts in the liver, lungs and less frequently in other organs. Surgical intervention is indicated in asymptomatic patients who do not respond to medical treatment or in case of hydatid disease complications [7].
During a hydatid cyst removal, an intact cyst should be removed. In case of rupture, there is a chance of severe anaphylactic reaction and daughter cysts implantation on nearby structures. But it is not always possible to remove the hydatid cysts intact, hence it is preferred to sterilize the cyst contents with various scolicidal agents e.g., hypertonic saline, formalin, hydrogen peroxide, silver nitrate, cetrimide, povidone-iodine, or absolute alcohol. Unfortunately, most of these scolicidal agents are not without complications. A few studies have shown that the use of hypertonic saline can lead to acute hypernatremia to a dangerous level, hence regular and frequent monitoring of serum sodium is mandatory during hypertonic saline lavage of the cyst cavity or peritoneal cavity after rupturing of hydatid cyst [8, 9].
The most common neurological complications due to acute hypernatremia, are in the form of brain matter shrinkage due to loss of intracellular water from brain cells which might lead to vascular damage and subdural hematomas [10]. Brain lesions in the form of Osmotic Demyelination Syndrome (previously known as central pontine and/or extra pontine myelinolysis) are thought to be due to rapid correction of preexisting hyponatremia [11–13]. Furthermore, it is thought that to counteract the rapid intracellular water loss during acute hypernatremia, brain cells tend to accumulate osmoles intracellularly as an adaptive response to minimize osmotic shrinkage. Unfortunately, this protective mechanism can lead to cerebral edema as the accumulated intracellular osmoles fail to dissipate at the same rate as that of hypernatremia correction [14–16].
It has been reported that in the case of acute hypernatremia, rapid correction of serum sodium at the rate of 1 mmol/l per hour can be done safely without neurological complications [2]. For rapid correction of serum sodium, peritoneal or hemodialysis can be done but these techniques have not shown any survival benefits over natriuresis combined with hypotonic fluid administration [3].
Regarding our case, early detection and rapid correction of acute hypernatremia at the rate of 1.5 mmol/l/h in the first 24 hours by using hypotonic fluids and natriuresis together with optimal management of anaphylactic shock, severe metabolic acidosis, and hyperglycemia were the hallmarks of our safe neurological outcome.
Our case of acute iatrogenic hypernatremia is unique in various aspects as follows:
1 — Our patient presented with complicated liver and lung hydatid cyst with a fistulous communication and anterior abdominal wall abscess. She had liver hydatid cyst removal surgery 6 years ago and an interventional radiological procedure (PAIR) 3 months ago.
2 — She was treated with hydatid cyst excision and peritoneal lavage for 40 to 60 minutes with 14.6% saline and her acute hypernatremia was immediately recognized post-operatively.
3 — She developed distributive shock just 1-hour postoperatively requiring epinephrine and norepinephrine infusions along with antihistamine and steroids. She was having a severe metabolic acidosis (normal anion gap) with pH 6.99 and HCO3- 8.9, and lactate of 3 in the immediate postoperative period.
4 — She developed intractable hyperglycemia requi-ring insulin infusion at high doses and rising WBC count (44,000) requiring resistant gram-negative and positive coverage in the form of meropenem and vancomycin post- operatively.
5 — In the immediate postoperative period she had an episode of generalized tonic-clonic seizure for approximately 20 to 30 seconds. Her CT and MRI brain was reported as normal. Clinically she became fully conscious, oriented in time, place, and person with no sensory or motor deficit in any of her four limbs.
Conclusions
The rate of sodium correction depends on how rapidly the hypernatremia developed and on the severity of symptoms. No major prospective studies in adults have been done to find the most appropriate and safe rate of correction, as most of the data is from the pediatric population. Postope-rative detection of acute hypernatremia, rapid correction of serum sodium at the rate of 1.5 mmol/l/h in the first 24 hours together with optimal treatment of distributive shock by using antihistamine, steroids, epinephrine, and norepinephrine is safe to avoid neurological complications. However, all efforts should be directed towards the prevention of severe hypernatremia [17, 18].
Received 27.03.2021
Revised 09.04.2021
Accepted 12.04.2021
Список литературы
1. Gullans S.R., Verbalis J.G. Control of brain volume during hyperosmolar and hypoosmolar conditions. Annu. Rev. Med. 1993. 44. 289-301.
2. Adrogue H.J., Madias N.E. Hypernatremia. N. Engl. J. Med. 2000. 342. 1493-1499.
3. Moder K.G., Hurley D.L. Fatal hypernatremia from exogenous salt intake: report of a case and review of the literature. Mayo Clin. Proc. 1990. 65. 1587-1594.
4. Goldszer R.C., Coodley E.L. Survival with severe hypernatremia. Arch. Intern. Med. 1979. 139. 936-937.
5. Ozcan P.E., Yavru A., Tugrul S., Akinci O., Erkan M., Ca-ker N. Iatrogenic hypernatremia during hydatid cyst operation. Ulus. Travma Acil Cerrahi Derg. 2003 Oct. 9(4). 291-293.
6. Dobato J.L., Barriga F.J., Pareja J.A., Vela L. Extra pontine myelinolysis caused by iatrogenic hypernatremia following rupture of hydatid cyst of the liver with an amnesic syndrome as a sequela. Rev. Neurol. 2000, Dec 1–15. 31(11). 1033-1035.
7. Taylor B.R., Langer B. Current surgical management of hepatic cyst disease. Adv. Surg. 1997. 31. 127-148.
8. Gage T.P., Vivian G. Hypernatremia after hypertonic saline irrigation of a hepatic hydatid cyst. Ann. Intern. Med. 1984. 101. 405.
9. Martinez Peralta C.A. A warning to surgeons who occasionally see hydatid cysts. Surgery. 1989. 105. 570.
10. Handy T.C., Hanzlick R., Shields L.B. et al. Hypernatremia and subdural hematoma in the pediatric age group: is there a causal relationship? J. Forensic Sci. 1999. 44. 1114-1118.
11. Wszolek Z.K., McComb R.D., Pfeiffer R.F. et al. Pontine and extra pontine myelinolysis following liver transplantation: relationship to serum sodium. Transplantation. 1989. 48. 1006-1012.
12. McComb R.D., Pfeiffer R.F., Casey J.H. et al. Late-ral pontine and extra pontine myelinolysis associated with hypernatremia and hyperglycemia. Clin. Neuropathol. 1989. 8. 284-288.
13. Ayus J.C., Armstrong D.L., Arieff A.I. Effects of hypernatremia in the central nervous system and its therapy in rats and rabbits. J. Physiol. 1996. 492. 243-255.
14. Soupart A., Penninckx R., Namias B. et al. Brain myelinolysis following hypernatremia in rats. J. Neuropathol. Exp. Neurol. 1996. 55. 106-113.
15. Lien Y.H., Shapiro J.I., Chan L. Effects of hypernatremia on organic brain osmoles. J. Clin. Invest. 1990. 85. 1427-1435.
16. Cserr H.F., DePasquale M., Nicholson C. et al. Extracellular volume decreases while cell volume is maintained by ion uptake in rat brain during acute hypernatremia. J. Physiol. 1991. 442. 277-295.
17. Kuzmanovska B., Kartalov A., Kuzmanovski I., Shosholcheva M., Jankulovski N., Gavrilovska-Brzanov A., Dimitrovski A., Cvetkovska E. Hypernatremia-induced Neurologic Complications After Hepatic Hydatid Cyst Surgery: Pretreat to Prevent. Med. Arch. 2019 Oct. 73(5). 356-358. doi: 10.5455/medarh.2019.73.356-358. PMID: 31819311; PMCID: PMC6885227.
18. Zeng R., Wu R., Lv Q., Tong N., Zhang Y. The association of hypernatremia and hypertonic saline irrigation in hepatic hydatid cysts: A case report and retrospective study [published correction appears in Medicine (Baltimore). 2018 Jan. 97(4). e9739] [published correction appears in Medicine (Baltimore). 2017 Dec. 96(52). e9528]. Medicine (Baltimore). 2017. 96(37). e7889. doi: 10.1097/MD.0000000000007889.
/124_2.jpg)

/123.jpg)
/123_2.jpg)
/124.jpg)