Статья опубликована на с. 173-178
Дефиниция. Согласно Всемирной организации здравоохранения (ВОЗ), лейшманиоз (ЛЗ) — это заболевание, связанное с низким социально-экономическим уровнем жизни, вызывающееся внутриклеточными простейшими, принадлежащими к роду Leishmania, которые распространяются трансмиссивным путем, через укусы флеботомных москитов [1].
Актуальность. Лейшмании — распространенная паразитарная инфекция, которая регистрируется в 98 странах мира. В планетарном масштабе ЛЗ поражено около 12 млн человек, из которых ежегодно умирает около 50 тыс. человек. При этом ежегодно регистрируется еще от 1,5 до 2 млн новых больных ЛЗ, из которых около полумиллиона случаев приходится на висцеральную форму ЛЗ (ВЛЗ) [1]. В новейшей истории Украины зарегистрировано порядка 40 случаев ЛЗ, из которых подавляющее большинство были завозными. Эндемичные случаи ЛЗ были зарегистрированы в Украине с 2008 по 2011 год в нескольких городах: Киеве (2008 г.), Львове (2008 г.), Сумах (2009 г.) и Харькове (2009–2011 гг.), особенностью эпидемиологического анамнеза было то, что все пациенты пребывали в АР Крым в разные периоды времени [2, 6]. Однако, по рекомендациям ВОЗ, наша страна относится к территориям со спорадическими случаями ЛЗ, несмотря на то, что имеются все составляющие эпидемического процесса: возбудитель, резервуар, а также переносчики инфекции.
Таким образом, ЛЗ не является исключительно тропической инфекцией и представляет реальную угрозу для общественного здоровья Украины.
Цель: улучшить диагностику причин лихорадки неясного происхождения (ЛНП) на основе описания клиники вероятного случая ВЛЗ Нового Света у ребенка раннего возраста.
Описание клинического случая
Девочка Т., 13.02.2014 г.р. (на момент заболевания 1 г. 7 мес.), этническая украинка, проживает со своими биологическими родителями в г. Днепропетровске.
По данным эпидемиологическго анамнеза, за 2 месяца до начала заболевания девочка со своей семьей вернулась в г. Днепропетровск из восточного штата Минас Жерайс (португал. Minas Gerais) Бразилии, где семья жила в течение 6 месяцев. Однократно за это время ребенок болел острой респираторной инфекцией, имели место укусы москитов. Девочка получила все прививки согласно национальному календарю вакцинации Украины, на диспансерном учете не состояла, реакции гиперчувствительности на медикаменты и пищу не наблюдались. Семейный анамнез не отягощен.
По данным анамнеза, заболевание началось 01.09.2015 остро, когда на фоне полного благополучия повысилась температура тела до гектических цифр, с потрясающими ознобами, которая купировалась на 2–3 часа после приема антипиретиков. Первую неделю заболевания ребенка лечил в амбулаторных условиях педиатр, который назначил амоксициллин/клавулановую кислоту (аугментин) внутрь в соответствующих возрасту дозах, антипиретики. Учитывая отсутствие эффекта от лечения, ребенок был госпитализирован в одну из детских больниц города, где продолжил терапию уже цефтриаксоном (лораксон) парентерально, в возрастной дозе в течение недели, а также однократно болюсом дексаметазон, инфузии кристаллоидов и антипиретики. Несмотря на проводимое лечение, девочка продолжала лихорадить, что явилось причиной ревизии антибактериальной химиотерапии и замены цефтриаксона на меропенем (меронем). Однако эскалация антибактериальной химиотерапии не привела к улучшению состояния ребенка: усилилась бледность кожи и слизистых, сохранялась гектическая лихорадка с ознобами, а также вялость и сонливость даже в период непродолжительной апирексии, увеличились размеры печени и селезенки, существенно возрастали лабораторные признаки системного воспалительного ответа (СВО) (табл. 1). Ребенок неоднократно консультировался врачами узких специальностей, по результатам этих консультаций был вынесен вердикт «дебют системного заболевания соединительной ткани» и рекомендовано назначение системной иммуносупрессивной терапии, где в качестве первого выбора рассматривались глюкокортикостероиды или альтернатива — гомологичный иммуноглобулин для внутривенного введения.
/174.jpg)
Миелограмма девочки по данным стернальной пункции (18.09.2015): препараты костного мозга гиперклеточные, индекс лейко-эритроцитарного соотношения сдвинут в сторону эритропоэза, отмечается незначительный диспоэз эритрона; созревание клеток нейтрофильного ряда в пределах нормы.
Данные инструментальных обследований ребенка, проведенных в Украине. Ультрасонография органов брюшной полости и забрюшинного пространства (17.09.2015) — гепатоспленомегалия, объемных образований и аномалий нет; рентгенограмма органов грудной клетки в прямой проекции (07.09.2015) — инфильтративных теней или признаков новообразований не обнаружено; обследование на малярию методом толстой капли (11.09.2015) — плазмодии не обнаружены; анализ крови на маркеры аутоиммунного процесса антинуклеарные и антимитохондриальные антитела (15.09.2015) — не обнаружены; анализ крови на вирус иммунодефицита человека (15.09.2015) — не обнаружен.
На 21-й день заболевания (21.09.2015) родители отказались от дальнейшего лечения в Украине и самостоятельно транспортировали ребенка в Турецкую Республику, где девочка была госпитализирована в инфекционное отделение (карта № 75079951, лечащий врач — проф. Metehen Özen) стамбульской клиники Acibadem Atakent Hastanesi с диагнозом: ЛНП (МКБ-10: R50.9 Fever, not identitied). Была вновь назначена химиотерапия тейкопланином сроком на 6 дней. В период нахождения в инфекционном отделении стамбульской клиники у девочки сохранялись гектическая лихорадка, бледность, увеличенные размеры печени и селезенки, усилился цитопенический синдром, что потребовало экстренной трансфузии эритроцитарной массы (22.09.2015). Указанная семиотика по-прежнему сопровождалась лабораторными признаками СВО — повышенным уровнем С-РП, ПКТ, гипертрансаминаземией и др. Эхокардиография (22.09.2015) патологии сердца не выявила. Повторная сонография в стамбульской клинике (22.09.2015) — гепатоспленомегалия, имеется незначительное количество свободной жидкости в брюшной полости. Проведенное серологическое исследование крови (21.09.2015) методом иммуноферментного анализа (ИФА) на присутствие антител класса М и G против Salmonella typhi и Salmonella paratyphi (реакция Видаля), Brucella, Borrelia burgdorferi — не обнаружены. По результатам иммунологического исследования крови (21.09.2015), содержание общих IgA — 82 (N 15–111) мг/дл, G — 789 (N 451–12001) мг/дл в пределах физиологической нормы, тогда как уровень IgM был незначительно повышен — 197 (N 35–184) мг/дл. Бактериологическое исследование (21.09.2015) кала, содержимого носоглотки и крови также не дало роста патогенных культур. Повторная стернальная пункция в стамбульской клинике (23.09.2015): препарат костного мозга гетерогенный, гиперклеточный. В эритроидном ростке дисплазия, мультинуклеарные ядра, присутствуют лизированные эритроциты. Атипичных клеток или бластных клеток не обнаружено. Амастиготных форм Leishmania не обнаружено. Анализ крови методом полимеразной цепной реакции (ПЦР) на присутствие ДНК Leishmania spp. (28.09.2015) — генетический материал Leishmania не обнаружен. Однако после видеоконференции 28.09.2015 (на 28-й день лихорадки) по системе Skype с бразильскими специалистами, которые расценили эту ситуацию как вероятный случай ВЛЗ Нового Света, турецкими врачами было принято решение начать пробное введение Amphotericin B liposomal (AmBisome) в дозе 3 мг/кг в сутки внутривенно через периферический катетер [8, 11]. На вторые сутки введения препарата температура еще сохранялась фебрильной, но к исходу третьих суток терапии AmBisome лихорадка стойко купировалась. Всего девочка получила 7-дневный курс инфузий AmBisome (общая доза препарата составила 21 мг/кг), по завершении которого в течение 10 дней улучшилось самочувствие девочки, сократились размеры печени и селезенки, нормализовался клеточный состав крови, исчезли параклинические признаки СВО. Ребенок выписан из инфекционного отделения клиники Acibadem Atakent Hastanesi с клиническим диагнозом «висцеральный лейшманиоз» (МКБ-10: В55.0 Viseral Leishmaniasis). По возвращении из Турции в г. Днепропетровск 14.11.2015 у девочки был проведен анализ крови методом ИФА, который не выявил специфических антител класса G к Leishmania spp. Девочка, по данным катамнестического наблюдения, в настоящее время здорова.
Дискуссия
Применяемая классификация заболевания построена на двух принципах: 1) географический — ЛЗ Старого (Евразия, Африка) Света и ЛЗ Нового (Южная и Центральная Америка) Света; 2) клинико-анатомический — кожная (локализованная, диффузная, рецидивирующая формы и пост-кала-азар), кожно-слизистый и висцеральный вариант ЛЗ [1]. Данная классификация очень удобна с практической точки зрения, так как позволяет определить эпидемиологию ЛЗ, сформулировать клинический диагноз и выбрать рациональную антипаразитарную химиотерапию. Анализируя представляемый случай, следует отметить, что семиотика заболевания ребенка подпадает под клинический диагноз ЛНП, которая определяется как патологическое состояние, основным проявлением которого является повышение температуры тела ≥ 38,3 °С на протяжении 3 и более недель, причина которой остается неизвестной после обследования с помощью общепринятых (рутинных) методов диагностики [4]. В национальном протоколе по диагностике ЛНП указано, что в качестве причин на долю инфекций приходится от 25 до 50 % [4]. Согласно указанному протоколу для верификации этиологии ЛНП следует также учитывать «географический, профессиональный маршруты», а при лабораторных обследованиях необходимо проводить анализы на ЛЗ путем выявления ДНК возбудителя [4].
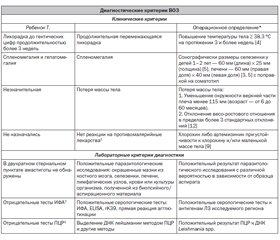
В связи с вышеизложенным основной ошибкой, если согласиться с диагнозом «висцеральная форма ЛЗ», явилась недооценка эпидемиологического анамнеза — длительное пребывание ребенка в штате Minas Gerais Бразилии, эндемичном по ЛЗ. Этот факт еще раз указывает на огромное значение тщательного сбора анамнеза, а также осведомленности врача об актуальной эпидемической ситуации в стране пребывания. Вместе с тем только эпидемиологические сведения при всей их важности обязаны должным образом подтверждаться клиническими признаками, инструментальными, лабораторными и специфическими паразитологическими исследованиями. Для унификации диагноза ВОЗ были предложены критерии ВЛЗ (табл. 2) [1].
/176.jpg)
Как видно из табл. 2, где сопоставляется семиотика заболевания девочки Т. с опорными диагностическими критериями ВЛЗ в соответствии с рекомендациями ВОЗ, лабораторного подтверждения диагноза этой паразитарной трансмиссивной инфекции нет. Вместе с тем следует учитывать, что наиболее уязвимой группой для ЛЗ-инфекции на любом континенте являются дети в возрасте до 5 лет, что обусловлено их анатомо-физиологическими особенностями и социальной зависимостью [1, 10]. Кроме того, в отличие от «резидентов» эндемичных зон, у лиц, временно проживающих на эндемичных по ЛЗ территориях, висцеральная форма заболевания начинается с внезапной лихорадки, выраженной слабости, недомогания, профузного потоотделения, быстрой потери веса и частых осложнений в виде тяжелой гемолитической анемии, что имело место у ребенка Т. [1]. При этом проведенные в дебюте заболевания в Украине обследования не выявили маркеров аутоиммунных и лимфопролиферативных заболеваний. Вместе с тем негативные результаты паразитологических и серологических методов исследования, являющиеся обязательными критериями согласно ВОЗ, ставят под сомнение диагноз ВЛЗ. Возможно, на результаты специфических лабораторных исследований повлияли следующие факторы. Во-первых, низкая чувствительность паразитологических методов диагностики. Классическим референс-тестом является визуализация амастиготных форм паразита посредством микроскопического исследования аспиратов тканей. Однако, несмотря на высокую специфичность прямой микроскопии, чувствительность этого способа относительно низкая и очень зависит от локуса обследования. Так, наибольшая чувствительность выделения ЛЗ методом прямой микроскопии имеет место при исследовании аспиратов селезенки (93–99 %), тогда как биоптатов костного мозга — 53–86 %, а лимфатических узлов еще меньше — 53–65 % [1]. Следует отметить, что в данном случае не применялось культивирование аспиратов/тканей органов, что значительно снизило чувствительность микроскопического метода диагностики. Существенным аспектом, влияющим на результаты прямого микроскопического исследования, являются навыки, знания врача-лаборанта, а также качество красителя. Во-вторых, серологические тесты, основанные на методах иммунохимического анализа (ИФА, ELISA, иммуноблоттинг в варианте вестерн-блотт). В Евразии в клинической лабораторной диагностике используют тест-системы на основе антигенов ЛЗ Старого Света, что, возможно, могло привести к ложноотрицательному результату в нашем случае. Указанное обстоятельство также могло повлиять на результаты исследования крови методом ПЦР, когда в праймерах использовались нуклеотидные последовательности Leishmania spp. Старого Света. При этом, по нашему мнению, более рациональным было бы провести анализ костномозгового биоптата на ДНК лейшманий методом ПЦР. Важным аргументом в пользу ЛЗ как возможной причины ЛНП является эффективная терапия липосомальным амфотерицином В. Вместе с тем показанием к назначению липосомального амфотерицина В также являются пациенты с нейтропенией и криптогенной (предполагаемой!) грибковой инфекцией [11]. Надо отметить, что в рассматриваемом клиническом случае девочка имела признаки снижения числа нейтрофилов, и эскалация антибактериальной химиотерапии без антимикотических препаратов резерва не привела к улучшению состояния здоровья ребенка.
Таким образом, при наличии ЛНП обследование на ЛЗ является рациональным, особенно для пациентов, посещавших субтропические или тропические регионы. Представленный клинический пример следует рассматривать как вероятный случай ВЛЗ Нового Света исходя из эпидемиологического анамнеза, длительной лихорадки с явлениями гепатоспленомегалии, анемии, гепатита и эффективности антипаразитарной химиотерапии липосомальным амфотерицином В.
Практические рекомендации
1. Диагноз ЛНП, особенно у лиц, посещавших суб- и тропические регионы, является предиктором для обследования не только на малярию, но и на иные трансмиссивные инфекции, в частности на ЛЗ.
2. Возможность профессиональной актуальной коммуникации с коллегами из Азии, Африки и Латинской Америки является важным аспектом рациональной диагностики и терапии тропических и эндемических инфекций.
3. Учитывая перспективы развития Украины, рационально создать специальную национальную систему по контролю и терапии тропических и эндемических инфекций.
Список литературы
1. Доклад № 949 «Борьба с лейшманиозом», 22–26 марта 2010 г. — К.: Комитет экспертов ВОЗ, 2010. — 243 с.
2. Колодий М.А. Лейшманиоз в Харьковской области / Колодий М.А. // Природно-очаговые инфекции: материалы Всеукраинской научно-практической конференции инфекционистов. — Ужгород, 2012. — С. 47-49.
3. Найдина Т.К. Нормальные возрастные размеры желчного пузыря, печени и поджелудочной железы у детей по данным эхографии / Найдина Т.К., Дворяковский И.В., Сугак А.Б. // Ультразвуковая и функциональная диагностика. — 2001. — № 4. — С. 57-59.
4. Приказ МЗ Украины № 626 «Клинический протокол оказания медицинской помощи больным с лихорадкой неизвестного происхождения» (действителен от 08.10.2007). — 5 c.
5. Пыков М.И. Детская ультразвуковая диагностика / М.И. Пыков, К.В. Ватолин. — М.: Видар, 2001. — 680 с.
6. Чемич Н.Д. Лейшманиоз: современные аспекты / Чемич Н.Д., Ильина Н.И., Захлебаева В.В., Шолохова С.Е. // Клиническая инфектология и паразитология. — 2013. — № 2(05). — С. 105-113.
7. Эпидемиология и статистика как инструменты доказательной медицины: [Пособие для студентов медицинских вузов, интернов, аспирантов, клинических ординаторов, врачей, менеджеров и организаторов здравоохранения] / Е.А. Корнышева, Д.Ю. Платонов, А.А. Родионов, А.Е. Шабашов. — 2-е изд. — Тверь, 2009. — 80 с.
8. AmBisome (amphotericin B) liposome for injection [Электронный ресурс]: база данных Astellas. — 2012. — P. 27. — Режим доступа к материалу: http://www.astellas.us/docs/ambisome.pdf.
9. Guidelines for the theatment of malaria / Third edition [WHO Library Cataloguing-in-Publication]. — Switzerland, 2015. — 266 p.
10. Sadiq M. Al-Hamash Mustansiriya Study of visceral leishmaniasis (kala-azar) in children of Iraq / Sadiq M. Al-Hamash Mustansiriya // Medical Journal. — 2012. — № 11(2). — P. 15-19.
11. Saravolatz L.D., Bern C., Adler-Moore J., Berenguer J., Boelaert M., Boer M., Davidson R.N., Figueras C., Gradoni L., Ka–fetzis D.A. et al. Liposomal Amphotericin B for the Treatment of Visceral Leishmaniasis / Saravolatz L.D. // Clinical Infectious Diseases. — 2006. — № 43(1). — P. 917-924.
12. WHO child growth standards and the identification of severe acute malnutrition in infants and children. — World Health Organization, United Nations Children’s Fund, 2009. — 11 p.
1. Control of the leishmaniasis: report of a meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010
2. Kolodij M.A. [Leishmaniasis in Kharkov region] Pry`rodno-oseredkovi infekciyi : materialy` Vseukrayins`koyi naukovo-prakty`chnoyi konferenciyi infekcionistiv. Uzhgorod. 2012;47–49. Ukrainian.
3. Najdy`na T.K., [Normal age-related dimensions of the gallbladder, liver and pancreas in children according to ultrasound]. Ul`trazvukovaya y` funkcy`onal`naya dy`agnosty`ka. 2001; 4: 57 — 59. Ukrainian.
4. Nakaz MOZ Ukrayiny vid 08.10.2007 №626 [Guidance for treatmen fever not identifyed]
5. Puikov MY, Vatolyn KV, autor; Puikov MY, editor. Det·skaya ul'trazvukovaya dyahnostyka [Ultrasound diagnosis for children]. Moscow: Vydar; 2001. 400 p. Russian.
6. Chemych ND, Yl'yna NY, Zakhlebaeva VV, Sholokhova SE. [Leishmaniasis: the modern aspects]. Klynycheskaya ynfektolohyya i parazytolohyya. 2013; №2(05); 105-113. Russian.
7. Kornusheva EA, Platonov DYu, Rodyonov AA, Shabashov AE,autors; Kornusheva EA, editor. Epydemyolohyya i statystyka kak instrumenty dokazatel'noy medytsyny: Posobye dlya studentov medytsynskykh VUZov, ynternov, aspyrantov, klynycheskykh ordynatorov, vrachey, menedzherov y orhanyzatorov zdravookhranenyya [Epidemiology and statistics as tools for evidence-based medicine: Manual for medical students, interns, graduate students, medical residents, doctors, managers and health administrators]. 2nd: rev., enl. Tver; 2009. 80p. Russian.
8. Astellas Database [Internet]. AmBisome (amphotericin B) liposome for injection [2012 May]. Available from: http://www.astellas.us/docs/ambisome.pdf
9. WHO Library Cataloguing-in-Publication [Internet]. Guidelines for the theatment of malaria (3rd.). 2015. Available from: http://www.who.int/malaria/publications/atoz/9789241549127/en/
10. Al-Hamash Mustansiriya SM. [Study of visceral leishmaniasis (kala-azar) in children of Iraq]. Mustansiriya Medical Journal. 2012; 11(2): 15-19.
11.Saravolatz LD, Bern C, Adler-Moore J, Berenguer J, Boelaert M, Boer M, Davidson RN, Figueras C, Gradoni L, Kafetzis DA et al. [Liposomal Amphotericin B for the Treatment of Visceral Leishmaniasis]. Clinical Infectious Diseases. 2006; 43(1):917-924.
12. World Health Organization, United Nations Children's Fund, autors; World Health Organization, editor. WHO child growth standards and the identification of severe acute malnutrition in infants and children. Switzerland; 2009; 11p.

/174.jpg)
/176.jpg)