Introduction
Since the mid-1950s, laparoscopy is applied during gynecological operations. This allowed reducing overall medical expenses, gave the possibility of rapid recovery with obtaining advantages in the field of psychosocial rehabilitation of patients and in the economic sense. It should be noted that for many patients the decisive factor is the cosmetic effect with minimal trauma to the skin, because, of course, a woman always remains a woman. Therefore, patients always want to be laparoscopically intervened, not laparotomic. Also, with laparoscopy, the number of pulmonary complications and bleeding decreased. Modern realities require laparoscopy, which includes more complex surgical procedures that led to the use of existing anesthetics with the greatest manageability and minimal side effects. The creation of pneumoperitoneum is an integral part of any laparoscopic procedure. The technique consists in insufflation of carbon dioxide for proper visualization of the abdominal cavity organs and for carrying out manipulation during interventions with great convenience. Of the negative moments, Trendelenburg position is added. The main effects are associated with an increase in intra-abdo–minal pressure, which leads to some negative effects. In the cardiovascular system, with a decrease in intra-abdominal pressure less than 15 mm Hg, venous return increases, which enables to increase cardiac output and blood pressure [1, 2]. According to the literature data, bradyarrhythmias leading to atrioventricular blockades are noted when the abdominal wall is stimulated by the introduction of carbon dioxide through the stimulation of vagal reflexes. Respiratory changes include a reduction in lung volume, the presence of basal atelectasis, increased intrapulmonary shunting, increased peak pressure and a reduced diaphragm excursion, there may also be a risk of endobronchial migration of the endotracheal tube [3].
Traditionally, general anesthesia with controlled ventilation was considered the only technique as a result of the effects of pneumoperitoneum, and various myths and facts prevented the use of regional anesthesia. The use of epidural anesthesia for laparoscopy has not gained popularity until recently due to the risk of aspiration and respiratory depression, which makes it less favorable for the patient in consciousness [4]. But in fact, the risk of aspiration on spontaneous breathing is less than with general anesthesia [5]. Recently, regional anesthesia has been considered as equally favorable in laparoscopic –operations [6, 7].
Of course, if surgery is performed under epidural ane–sthesia, after 1.5 hours most anesthesiologists perform tracheal intubation with the transition to artificial ventilation, which is associated, according to the literature, with the patient’s regurgitation. It was very interesting to study the possibility of preserving spontaneous breathing during laparoscopic interventions for up to five hours or more. Since in this case we are able to obtain such positive effects as the earlier restoration of cognitive functions, then in the future it allows for an earlier discharge of patients with the achievement of economic benefits by reducing the burden on medical personnel, the absence of the need for transfer of patients to the intensive care unit and significant reduction of the patient’s stay in the hospital.
Stress reactions to surgical trauma include activation of the hypothalamic-pituitary-adrenal system and the release of inflammatory cytokines, in particular interleukin-6 (IL-6) and IL-8 [8]. The concentration of inflammatory cytokines IL-6 and IL-8, which are powerful activators of neutrophils, increases within 30–60 minutes after the beginning of surgery, reaches a maximum in 4 hours and remains elevated for 48–72 hours after the operation. The values of cytokines reflect the degree of tissue trauma, so their secretion is lowest in less invasive and traumatic procedures.
Epidural anesthesia, according to literature data, was combined appropriately with general anesthesia –using inhaled anesthetics [9], which leads to a decrease in the stress response. At the same time, the duration of gynecological operations in cancer patients conside–ring the appearance of technical complications may be unpredictably increased to five hours and even more. To maintain spontaneous breathing with comfortable anesthesia using epidural anesthesia for many hours of surgery, it is necessary to study more thoroughly the possibility of conducting it with advanced therapy of possible complications and a comfortable state of patients. According to our data and world literature, propofol as a general anesthetic is an alternative to inhalation anesthetics in terms of the rate of recovery of cognitive functions [10, 11]. Although propofol is believed to lead to respiratory depression, its infusion at a rate of 5 mg/kg/h with a blood concentration of 2000–2500 ng/ml is clinically sufficient to maintain spontaneous breathing. For sedation, thiopental sodium is also used instead of propofol, which is close to the rate of recovery of cognitive functions. Therefore, taking into account the above-mentioned positive points, the use of epidural anesthesia with sedation on spontaneous breathing is more promising for long-term surgical interventions.
Purpose: study and justification of the expediency of using epidural anesthesia with sedation on spontaneous breathing in cancer patients during prolonged gynecological laparoscopic interventions to provide anesthesia with advanced therapy of possible complications and obtain a more comfortable condition of patients.
Materials and methods
After receiving the approval of the ethics committee and informed consent, a prospective, randomized, double-blind study was conducted on the clinical basis of the SI “Grigoriev Institute for Medical Radio–logy of the National Academy of Medical Sciences of Ukraine”. The study involved 64 patients with ovarian, uterine and cervical cancer with gynecological laparoscopic interventions, ASA (American Society of Anaesthesiologists) I and II, who were stratified depending on the type of anesthesia: group A (control; n = 25) — combined general anesthesia with epidural analgesia according to standard protocols, and group B (n = 39) — epidural anesthesia on spontaneous breathing with sedation. Physical parameters of patients: age — 62.6 ± 2.1 years, body weight — 78.8 ± 2.2 kg, body mass index — 27.2 ± 0.9 kg/m2.
All patients underwent premedication: 0.005–0.008 mg/kg atropine and 0.5–1.0 mg dexketoprofen 2 ml intramuscularly 30 minutes before the surgery. In the ope–rating room, intravenous ondansetron hydrochloride dihydrate 4 ml was injected. Continuous monitoring of vital parameters (electrocardiogram, pulse oximetry (SpO2) and noninvasive measurement of systolic and diastolic blood pressure) was also performed in the operating room.
In group A slow injection (4–5 ml every 2–3 min) was performed under local analgesia (2 ml of 2% lidocaine) into the epidural space at the Th9-Th10 level — local anesthetic bupivacaine 0.5% at a dose of 23–25 ml with 0.05 mg of fentanyl just before induction of general ane–sthesia. General anesthesia was induced with thiopental sodium 4–6 mg/kg or diprofol 1.6–2 mg/kg, diaze–pam 0.1–0.2 mg/kg intravenously. The patients underwent muscle relaxation with a non-depolarizing muscle rela–xant with an intermediate-acting atracurium besylate at a dose of 0.5–0.6 mg/kg. Tracheal intubation was carried out, then maintenance doses of thiopental sodium of 1.5–2 mg kg or diprofol 0.5–0.8 mg/kg every 20 minutes and atracurium bezylate 0.26 mg/kg every 30 minutes were administered.
In group B, under local analgesia, a slow (4–5 ml every 2–3 minutes) injection of a local anesthetic 0.5% of bupivacaine in a dose of 23–25 ml with 0.05 mg of fentanyl was performed at the level of Th9-Th10. Further sedation was carried out once with diazepam administration at a dose of 0.07–0.1 mg/kg and a maintenance dose of intravenous dropping thiopental sodium 2.8–3.2 mg/kg/hr or diprofol 2.7–3.8 mg/kg/h. Starting from 150 minutes after the beginning of the operation, fentanyl was injected intravenously at a dose of 25 μg every 30 minutes.
The pressure of intra-abdominal CO2 was maintained between 12 and 15 mm Hg and did not exceed 15 mm Hg. According to the literature, after the end of laparoscopic surgery and anesthesia, pain of various severity in the right shoulder often arises in patients as a manifestation of irritation of the vagal and sympathetic nerve plexuses in pneumoperitoneum, but in our study, during the operation we did not perform a right-sided superficial blockade of the cervical plexus and terminal anesthesia of the diaphragm surface.
To measure cytokine concentrations, blood samples were obtained before surgery and 4 and 24 hours after it. The blood was placed into EDTA tubes and centrifuged at 3000 rpm for 5 minutes at 4 °C immediately after sampling. After this, the plasma was stored at –80 °C until analysis [12]. Plasma concentrations of IL-6 and IL-8 were measured using a commercial quantitative ELISA kit.
The neuromuscular block was monitored based on a subjective evaluation by the operating gynecologist and using Datex relaxograph. The standard for modern mo–nitors was a special stimulation mode referred to as TOF (train-of-four). The essence of the technique is that a series of four short pulses is fed at intervals of 0.5 second.
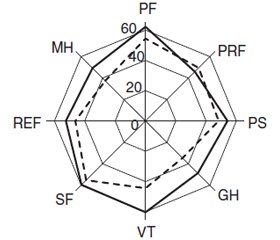
A study of the general health-related quality of life was carried out with the help of the standard validated Short Questionnaire for Health Status Assessment SF-36, using the Evidence methodology (the quality of life is directly proportional to the score) in a shortened follow-up period of up to 1 week. Based on the results of the analysis of the answers to its questions, a socio-psychological profile of a patient [13] was formed, which includes the following parameters: physical functioning (PF), physical role functioning (PRF), pain severity (PS), general health (GH), vitality (VT), social functioning (SF), emotional role functioning (ERF), mental health (MH). Parameters of the overall quality of life were assessed on a 100-point scale.
A preliminary evaluation of the indicators distribution was carried out by a visual method and using the Shapiro-Wilk criterion. The statistical processing of the results was carried out by means of the Statistica 10 software package, using the Wilcoxon-Mann-Whitney test. For each sample, the median (Me), the upper and lower quartiles [Q1; Q3] were calculated. The statistical significance of differences in the indices of the experimental and the comparison group was evaluated according to the Mann-Whitney U test. The results obtained are given in the form of an arithmetic mean-mean-square deviation. Differences were considered statistically significant at p < 0.05 or tended to be reliable at 0.1 > p > 0.05.
Results
The duration of operations was 252.6 ± 53.5 min. No patient was excluded from the study. Group B, in which for sedation propofol or thiopental sodium were admi–nistered depending on the clinical signs of anesthesia to provide superficial sleep, never required switching to auxiliary or artificial ventilation of the lungs.
In our study, we preoperatively administered ondansetron and conducted a slow administration of bupi–vacaine with epidural anesthesia, so vomiting was noted only in one patient in group B three minutes after the administration of the anesthetic. But in the future du–ring anesthesia, there was no repeated vomiting or other complications. In three cases, there was nausea, but it was rather a manifestation of lowering blood pressure. Although evaluated blood loss was 442.6 ± 203.5 ml, none of the patients needed the use of sympathomimetics or blood transfusion. Stabilization of blood pressure was achieved by preoperative water loading in the volume of 800–1300 ml and the introduction of colloidal solutions.
At the same time, when performing surgeries in patients from group B, relaxation compared to group A was sufficient according to the subjective evaluation of the operating gynecologist and the results of instrumental monitoring of the completeness of the neuromuscular block on the Datex relaxograph.
Respiratory depression significant for the violation of ventilation from sedation did not occur, since conducting an epidural anesthesia at the Th9-Th10 level at a dose of 23–25 ml does not affect the function of the diaphragm. According to the literature data, transperitoneal absorption of CO2 may be the main cause of hypercarbia, and the hypercarbia is not attributed to the increase in the dead space/tidal volume ratio; and oxygenation is not impaired during pneumoperitoneum [14]. At the same time, in the postoperative period, there were no respiratory disorders and complications in the form of bronchitis or pneumonia (in many respects, this is due to the use of preventive antibiotic therapy).
No one reported the absence or one-sidedness of the epidural block, which indicates a sufficient qualification of anaesthesiologists. All patients had spontaneous breathing with oxygen-enriched air (O2 — 4–4.5 l/min). According to the pulse oximetry, the saturation (SpO2) during the operative intervention was within the range of 96–100 %. The respiratory rate under the operation conditions is within the range of 12–16 breaths per minute.
Discussion
Preoperative levels of cytokines are the same, their level peaked in 4 hours, decreasing almost 2 times in 24 hours after the surgery in all groups. The findings did not reveal a statistically significant difference between the physiological group and other groups in the levels of IL-6 and IL-8. However, after 4 and 24 hours, IL-6 and IL-8 levels were significantly lower in group B compared to group A (p < 0.05, Fig. 1 and Fig. 2, respectively, for IL-6 and IL-8).
During and after the end of laparoscopic surgery and anesthesia, patients report pain of different intensity in the right shoulder often arises that is associated with a gas residue in the subdiaphragm space that stimulates the diaphragmatic nerve. But in our studies, no such complaints have ever been noted, which may be due to the introduction of intravenous fentanyl in the B group at a dose of 25 μg every 30 min after 150 minutes. Therefore, in our patients, right-sided superficial blockade of the cervical plexus and terminal anesthesia of the surface of the diaphragm were not performed.
Evaluation of the quality of life associated with the health of patients during long hours of gynecological la–paroscopic interventions showed higher values in group B, the contingent of which was used epidural anesthesia with sedation (Fig. 3).
As we can see from the Fig. 3, the evaluation of the quality of life during the many hours of gynecological laparoscopic interventions revealed higher values in group B except for role physical functioning with the reliability of differences of the changes in the indices at p < 0.05.
Conclusions
1. Our anesthesia, epidural anesthesia with sedation on spontaneous breathing, can be successfully used for many patients, because despite prolonged gynecological laparoscopic interventions, no complications were found in our studies.
2. Under epidural anesthesia with preservation of spontaneous breathing, we are able to conduct anesthesia, comfortably because according to the quality of life evaluation, during prolonged gynecological laparoscopic interventions, better indicators were found in comparison with combined anesthesia (р < 0.05).
3. According to intra- and postoperative survey, humeral syndrome didn’t develop; therefore, right-sided superficial blockade of the cervical plexus and terminal anesthesia of the diaphragm surface are not used. Application of preoperative water load in the volume of 800–1300 ml and the introduction of colloid solutions allows maintaining effectively the hemodynamics of patients during laparoscopic interventions, optimizing the effect on blood pressure and heart rate.
4. Anesthesia of a patient without traditional anesthesia with inherent deficiencies significantly shortens the patient’s recovery period after surgery, subsequently have psychoemotional and economic benefits, since immediately after the operation the patient is in a comfortable state, in the evening after the surgery can get up without help.
Conflicts of interests. Authors declare no conflicts of interests that might be construed to influence the results or interpretation of their manuscript.
The research is a fragment of the research work “Development of an algorithm for individualizing the tactics of intensive care in cancer patients after multiple organ procedures” (number of state registration 0117U001049), SI “Grigoriev Institute for Medical Radiology of the National Academy of Medical Sciences of Ukraine” (director — prof. M.V. Krasnoselskiy).
Information on contribution of each author:
M.V. Krasnoselskiy — concept and design of the research.
Ye.M. Krutko — design of the research, data collection.
M.V. Shulga — data collection and processing.
Ye.V. Shulga — analysis of the received data, collection of materials and writing the text.
V.G. Seredenko — writing the text.
Список литературы
1. Gutt C.N., Oniu T., Mehrabi A., Schemmer P., Kashfi A., Kraus T. et al. Circulatory and respiratory complications of carbon dioxide insufflation // Dig. Surg. 2004; 21(2): 95-105. doi: 10.1159/000077038.
2. Zuckerman R.S., Heneghan S. The duration of hemodynamic depression during laparoscopic cholecystectomy // Surg. Endosc. 2002 Aug; 16(8): 1233-6. doi: 10.1007/s00464-001-9152-0.
3. Rauh R., Hemmerling T.M., Rist M., Jacobi K.E. Influence of pneumoperitoneum and patient positioning on respiratory system compliance // J. Clin. Anesth. 2001 Aug; 13(5): 361-5. PMID: 11498317.
4. Bajwa S.J., Kulshrestha A. Anaesthesia for laparoscopic surgery: general vs regional anaesthesia // J. Minim. Access Surg. 2016 Jan-Mar; 12(1): 4-9. doi: 10.4103/0972-9941.169952.
5. Mazdisnian F., Palmieri A., Hakakha B., Hakakha M., Cambridge C., Lauria B. et al. Office microlaparoscopy for female sterilization under local anesthesia. A cost and clinical analysis // J. Reprod. Med. 2002 Feb; 47(2): 97-100. PMID: 11883359.
6. Thwaites A., Edmends S., Smith I. Inhalation induction with sevoflurane: a double-blind comparison with propofol // Br. J. Anaesth. 1997 Apr; 78(4): 356-61. PMID: 9135350.
7. Iwama H., Obara S., Ozawa S., Furuta S., Ohmizo H., Watanabe K. et al. A survey of combined epidural-propofol ane–sthesia with noninvasive positive pressure ventilation as a minimally invasive anesthetic protocol // Med. Sci. Monit. 2003 Jul; 9(7): CR316-23. PMID: 12883451.
8. Lin E., Calvano S.E., Lowry S.F. Inflammatory cytokines and cell response in surgery // Surgery. 2000 Feb; 127(2): 117-26. doi: 10.1067/msy.2000.101584.
9. Ozcan S., Ozer A.B., Yasar M.A., Erhan O.L. Effects of combined general anesthesia and thoracic epidural analgesia on cytokine response in patients undergoing laparoscopic cholecystectomy // Niger. J. Clin. Pract. 2016 Jul-Aug; 19(4): 436-42. doi: 10.4103/1119-3077.183308.
10. Zabolotskikh I., Trembach N. Safety and efficacy of combined epidural/general anesthesia during major abdominal surgery in patients with increased intracranial pressure: a cohort study // BMC Anesthesiol. 2015, May 15; 15: 76. doi: 10.1186/s12871-015-0056-2.
11. Pei L., Tan G., Wang L., Guo W., Xiao B., Gao X. et al. Comparison of combined general-epidural anesthesia with general anesthesia effects on survival and cancer recurrence: a meta-ana–lysis of retrospective and prospective studies // PLoS One. 2014, Dec 30; 9(12): e1146-67. doi: 10.1371/journal.pone.0114667.
12. Xu Q., Zhang H., Zhu Y.M., Shi N.J. Effects of combined general/epidural anesthesia on hemodynamics, respiratory function, and stress hormone levels in patients with ovarian neoplasm undergoing laparoscopy // Med. Sci. Monit. 2016, Nov 8; 22: 4238-46. doi: 10.12659/MSM.897430.
13. Karlsen R.V., Frederiksen K., Larsen M.B., von Heymann-Horan A.B., Appel C.W., Christensen J. et al. The impact of a breast cancer diagnosis on health-related quality of life. A prospective comparison among middle-aged to elderly women with and without breast cancer // Acta Oncol. 2016 Jun; 55(6): 720-27. doi: 10.3109/0284186X.2015.1127415.
14. Ishikawa S., Makita K., Sawa T., Toyooka H., Amaha K. Ventilatory effects of laparoscopic cholecystectomy under general anesthesia // J. Anesth. 1997 Sep; 11(3): 179-183. doi: 10.1007/BF02480034.

/166-1.jpg)