Журнал «Боль. Суставы. Позвоночник» Том 13, №3, 2023
Вернуться к номеру
Рекомендації щодо діагностики, профілактики та лікування постменопаузального остеопорозу
Авторы: Григор’єва Н.В. (1), Коваленко В.М. (2), Корж М.О. (3), Татарчук Т.Ф. (4), Дєдух Н.В. (1), Страфун С.С. (5), Дубоссарська З.М. (6), Проценко Г.О. (2), Калашніков А.В. (5), Мусієнко А.С. (1), Регеда С.І. (7), Єфіменко О.О. (7, 8), Чайківська Е.Ф. (9)
(1) — Державна установа «Інститут геронтології імені Д.Ф. Чеботарьова Національної академії медичних наук України», м. Київ, Україна
(2) — Державна установа «Національний науковий центр «Інститут кардіології, клінічної та регенеративної медицини імені академіка М.Д. Стражеска Національної академії медичних наук України», м. Київ, Україна
(3) — ДУ «Інститут патології хребта та суглобів імені проф. М.І. Ситенка Національної академії медичних наук України», м. Харків, Україна
(4) — Державна установа «Інститут педіатрії, акушерства і гінекології імені академіка О.М. Лук’янової Національної академії медичних наук України», м. Київ, Україна
(5) — Державна установа «Інститут травматології та ортопедії Національної академії медичних наук України», м. Київ, Україна
(6) — Дніпровський державний медичний університет Міністерства охорони здоров’я України, м. Дніпро, Україна
(7) — ДНУ «Центр інноваційних медичних технологій Національної академії наук України», м. Київ, Україна
(8) — КНП «Київський міський клінічний ендокринологічний центр», м. Київ, Україна
(9) — Львівський державний медичний університет імені Данила Галицького, м. Львів, Україна
Рубрики: Ревматология, Травматология и ортопедия
Разделы: Справочник специалиста
Версия для печати
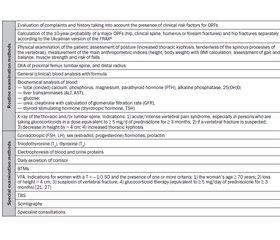
Актуальність. Постменопаузальний остеопороз (ПМП ОП), який виникає внаслідок дефіциту естрогенів у жінок після настання менопаузи, — найбільш поширений тип системного остеопорозу. Українські рекомендації щодо його менеджменту потребують перегляду у зв’язку з отриманням останніми роками нових даних і результатів високоякісних досліджень. Мета дослідження — на основі аналізу сучасних літературних джерел розробити Рекомендації щодо діагностики, профілактики та лікування постменопаузального остеопорозу задля поліпшення обізнаності медичної спільноти України. Методологія. Для розробки Рекомендацій була створена експертна група з 13 провідних українських вчених різного фаху, які провели ретельний огляд сучасних літературних джерел щодо цієї проблеми, за допомогою системи GRADE оцінили рівень наявних доказів, запропонували 15 положень Рекомендацій та проголосували за них. Результати. Ці Рекомендації містять розділи щодо діагностики та диференційної діагностики ПМП ОП, оцінки ризику остеопоротичних переломів, ролі біохімічних маркерів кісткового ремоделювання в менеджменті ПМП ОП, сучасних стратегій антиостеопоротичного лікування. Висновки. Українські Рекомендації щодо діагностики, профілактики та лікування ПМП ОП, які містять 15 основних положень, розроблених на ґрунті ретельного аналізу й синтезу сучасних літературних даних щодо цього питання, є важливим інструментом для менеджменту ПМП ОП і рекомендовані до використання у практичній охороні здоров’я лікарями різного фаху.
Background. Postmenopausal osteoporosis (PMO), which is developed due the estrogen deficiency in women after menopause, is the most common type of systemic osteoporosis. The latest Ukrainian recommendation for its management requires revision due to new data from high-quality research performed in recent years. The purpose was to develop a guideline on the diagnosis, prevention, and treatment of PMO based on an analytical analysis of modern literary sources in order to improve the awareness of the medical community of Ukraine. Methodology. To develop the guideline, an expert group of 13 leading Ukrainian scientists of various specialties was created who conducted a thorough review of modern literature on this topic, assessed the level of existing evidence using the GRADE system, proposed and voted on 15 recommendations of the guideline. Results. The guideline contains chapters on diagnosis and differential diagnosis of PMO, assessment of the osteoporotic fracture risk, the role of bone turnover markers in the management of PMO, and modern strategies of antiosteoporotic treatment. Conclusions. The Ukrainian guideline on the diagnosis, prevention, and treatment of PMO, which contains 15 main recommendations, created on the basis of a thorough analysis and synthesis of modern literature data, is an important tool for the management of PMO and is recommended by Ukrainian Association of Osteoporosis for use in Ukrainian medical community.
рекомендації; постменопаузальний остеопороз; діагностика; профілактика; лікування
guideline; recommendations; Ukraine; postmenopausal osteoporosis; diagnostics; prevention; treatment
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- International Osteoporosis Foundation. About Osteoporosis. Available from: https://www.osteoporosis.foundation/health-professionals/about-osteoporosis. Accessed: 2023 Aug 25.
- Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993 Jun;94(6):646-50. doi: 10.1016/0002-9343(93)90218-e.
- WHO. Disorders of bone density and structure. In: International Statistical Classification of Diseases and Related Health Problems 10th Revision; Chapter XIII: Diseases of the musculoskeletal system and connective tissue. M80-M85. Available from: https://icd.who.int/browse10/2019/en#/M80. Accessed: 2023 Aug 30.
- Akkawi I, Zmerly H. Osteoporosis: Current Concepts. Joints. 2018 Jun 14;6(2):122-127. doi: 10.1055/s-0038-1660790.
- WHO. Menopause. Available from: https://www.who.int/news-room/fact-sheets/detail/menopause. Accessed: 2023 Aug 30.
- Hill K. The demography of menopause. Maturitas. 1996 Mar;23(2):113-27. doi: 10.1016/0378-5122(95)00968-x.
- Kanis JA, Norton N, Harvey NC, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos. 2021 Jun 2;16(1):82. doi: 10.1007/s11657-020-00871-9.
- Povoroznyuk VV, Dzerovich NI, Karasevska TA. Bone mineral density in Ukrainian women of different ages. Diseases of the musculoskeletal system in people of different ages (selected lectures, reviews, articles); Vol 3. Kyiv: 2014. pp. 38-48.
- Verner IE, editor. Statistical yearbook 2021. Kyiv: State service of statistics of Ukraine; 2022. 447 p.
- Povoroznyuk VV, Grygorieva NV, Kanis JA, et al. Epidemiology of Hip Fractures in Two Regions of Ukraine. J Osteoporos. 2018 Jun 3;2018:7182873. doi: 10.1155/2018/7182873.
- Povoroznyuk VV, Grygorieva NV, Kanis JA, et al. Epidemiology of hip fracture and the development of FRAX in Ukraine. Arch Osteoporos. 2017 Dec;12(1):53. doi: 10.1007/s11657-017-0343-2.
- Eastell R, O'Neill TW, Hofbauer LC et al. Postmenopausal osteoporosis. Nat Rev Dis Primers. 2016 Sep 29;2:16069. doi: 10.1038/nrdp.2016.69.
- Bhatnagar A, Kekatpure AL. Postmenopausal Osteoporosis: A Literature Review. Cureus. 2022 Sep 20;14(9):e29367. doi: 10.7759/cureus.29367.
- Brown JP. Long-Term Treatment of Postmenopausal Osteoporosis. Endocrinol Metab (Seoul). 2021 Jun;36(3):544-552. doi: 10.3803/EnM.2021.301.
- Kanis JA, Cooper C, Rizzoli R, Reginster JY; Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019 Jan;30(1):3-44. doi: 10.1007/s00198-018-4704-5.
- Kovalenko VM, Povoroznyuk VV, Bortkevich OP and others. Guidance for diagnostic, prevention and management of osteoporosis in postmenopausal women. Ukrainian Journal of Rheumatology. 2009;(3):23-39.
- World Health Organization. WHO handbook for guideline development, 2nd ed. Switzerland: World Health Organization; 2014. 167 p.
- Guyatt GH, Oxman AD, Vist GE, et al; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 26;336(7650):924-6. doi: 10.1136/bmj.39489.470347.AD.
- Varyvonchyk DV, Hoyda NG, Horbenko GV, et al., authors; Ross G, Novichkova O, editors. Guide for developers of clinical recommendations/medical standards. Kyiv: NICARE; 2006. 166 p.
- Brouwers MC, Kho ME, Browman GP, et al.; AGREE Next Steps Consortium. AGREE II: Advancing guideline development, reporting and evaluation in healthcare. CMAJ 2010;182:E839-842.
- ISDC. 2019 ISCD Official Positions. Adults. Available from: https://iscd.org/learn/official-positions/adult-positions. Accessed: 2023 Aug 30.
- Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008 Mar;42(3):467-75. doi: 10.1016/j.bone.2007.11.001.
- Kanis JA, Johnell O, Oden A, et al. The use of multiple sites for the diagnosis of osteoporosis. Osteoporos Int. 2006;17(4):527-34. doi: 10.1007/s00198-005-0014-9.
- Leslie WD, Lix LM, Tsang JF, Caetano PA; Manitoba Bone Density Program. Single-site vs multisite bone density measurement for fracture prediction. Arch Intern Med. 2007 Aug 13-27;167(15):1641-7. doi: 10.1001/archinte.167.15.1641.
- Osteopenia: International Classification of Diseases for Mortality and Morbidity Statistics, 11th Revision, v2023-01. Available from: https://www.findacode.com/icd-11/block-611604654.html. Accessed: 2023 Aug 30.
- Kendler DL, Compston J, Carey JJ, Wu CH, Ibrahim A, Lewiecki EM. Repeating Measurement of Bone Mineral Density when Monitoring with Dual-energy X-ray Absorptiometry: 2019 ISCD Official Position. J Clin Densitom. 2019 Oct-Dec;22(4):489-500. doi: 10.1016/j.jocd.2019.07.010.
- Borges JLC, Sousa da Silva M, Ward RJ, Die–mer KM, Yeap SS, Lewiecki EM. Repeating Vertebral Fracture Assessment: 2019 ISCD Official Position. J Clin Densitom. 2019 Oct-Dec;22(4):484-488. doi: 10.1016/j.jocd.2019.07.005.
- Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996 May 18;312(7041):1254-9. doi: 10.1136/bmj.312.7041.1254.
- Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005 Jul;20(7):1185-94. doi: 10.1359/JBMR.050304.
- Siris ES, Miller PD, Barrett-Connor E, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001 Dec 12;286(22):2815-22. doi: 10.1001/jama.286.22.2815.
- Eriksen EF. Treatment of osteopenia. Rev Endocr Metab Disord. 2012 Sep;13(3):209-23. doi: 10.1007/s11154-011-9187-z.
- Compston J, Cooper A, Cooper C, et al.; National Osteoporosis Guideline Group (NOGG). UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017 Dec;12(1):43. doi: 10.1007/s11657-017-0324-5.
- LeBoff MS, Greenspan SL, Insogna KL, et al. The clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2022 Oct;33(10):2049-2102. doi: 10.1007/s00198-021-05900-y.
- Salari N, Darvishi N, Bartina Y, et al. Global prevalence of osteoporosis among the world older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021 Nov 13;16(1):669. doi: 10.1186/s13018-021-02821-8.
- Aspray TJ, Hill TR. Osteoporosis and the Ageing Skeleton. Subcell Biochem. 2019;91:453-476. doi: 10.1007/978-981-13-3681-2_16.
- Bouxsein ML, Eastell R, Lui LY, et al.; FNIH Bone Quality Project. Change in Bone Density and Reduction in Fracture Risk: A Meta-Regression of Published Trials. J Bone Miner Res. 2019 Apr;34(4):632-642. doi: 10.1002/jbmr.3641.
- Svejme O, Ahlborg HG, Nilsson JЕ, Karlsson MK. Low BMD is an independent predictor of fracture and early menopause of mortality in post-menopausal women--a 34-year prospective study. Maturitas. 2013 Apr;74(4):341-5. doi: 10.1016/j.maturitas.2013.01.002.
- Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004 Aug;35(2):375-82. doi: 10.1016/j.bone.2004.03.024.
- Johnson NA, Stirling ER, Divall P, Thompson JR, Ullah AS, Dias JJ. Risk of hip fracture following a wrist fracture-A meta-analysis. Injury. 2017 Feb;48(2):399-405. doi: 10.1016/j.injury.2016.11.002.
- Kanis JA, Johansson H, Oden A, et al. A family history of fracture and fracture risk: a meta-analysis. Bone. 2004 Nov;35(5):1029-37. doi: 10.1016/j.bone.2004.06.017.
- De Laet C, Kanis JA, Odén A, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005 Nov;16(11):1330-8. doi: 10.1007/s00198-005-1863-y.
- Kaze AD, Rosen HN, Paik JM. A meta-analysis of the association between body mass index and risk of vertebral fracture. Osteoporos Int. 2018 Jan;29(1):31-39. doi: 10.1007/s00198-017-4294-7.
- Kanis JA, Johnell O, Oden A, et al. Smoking and fracture risk: a meta-analysis. Osteoporos Int. 2005 Feb;16(2):155-62. doi: 10.1007/s00198-004-1640-3.
- Shen GS, Li Y, Zhao G, et al. Cigarette smoking and risk of hip fracture in women: a meta-analysis of prospective cohort studies. Injury. 2015 Jul;46(7):1333-40. doi: 10.1016/j.injury.2015.04.008.
- Kanis JA, Johansson H, Johnell O, et al. Alcohol intake as a risk factor for fracture. Osteoporos Int. 2005 Jul;16(7):737-42. doi: 10.1007/s00198-004-1734-y.
- Asoudeh F, Salari-Moghaddam A, Larijani B, Esmaillzadeh A. A systematic review and meta-analysis of prospective cohort studies on the association between alcohol intake and risk of fracture. Crit Rev Food Sci Nutr. 2022;62(20):5623-5637. doi: 10.1080/10408398.2021.1888691.
- Ke Y, Hu H, Zhang J, et al. Alcohol Consumption and Risk of Fractures: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv Nutr. 2023 Jul;14(4):599-611. doi: 10.1016/j.advnut.2023.03.008.
- Cheraghi Z, Doosti-Irani A, Almasi-Hashiani A, et al. The effect of alcohol on osteoporosis: A systematic review and meta-analysis. Drug Alcohol Depend. 2019 Apr 1;197:197-202. doi: 10.1016/j.drugalcdep.2019.01.025.
- Zhou J, Liu B, Qin MZ, Liu JP. Fall Prevention and Anti-Osteoporosis in Osteopenia Patients of 80 Years of Age and Older: A Randomized Controlled Study. Orthop Surg. 2020 Jun;12(3):890-899. doi: 10.1111/os.12701.
- Anagnostis P, Siolos P, Gkekas NK, et al. Association between age at menopause and fracture risk: a systematic review and meta-analysis. Endocrine. 2019 Feb;63(2):213-224. doi: 10.1007/s12020-018-1746-6.
- Xue AL, Wu SY, Jiang L, Feng AM, Guo HF, Zhao P. Bone fracture risk in patients with rheumatoid arthritis: A meta-analysis. Medicine (Baltimore). 2017 Sep;96(36):e6983. doi: 10.1097/MD.0000000000006983.
- Chen B, Cheng G, Wang H, Feng Y. Increased risk of vertebral fracture in patients with rheumatoid arthritis: A meta-analysis. Medicine (Baltimore). 2016 Nov;95(45):e5262. doi: 10.1097/MD.0000000000005262.
- Jin S, Hsieh E, Peng L, et al. Incidence of fractures among patients with rheumatoid arthritis: a systematic review and meta-analysis. Osteoporos Int. 2018 Jun;29(6):1263-1275. doi: 10.1007/s00198-018-4473-1.
- Napoli N, Conte C. Bone fragility in type 1 diabetes: new insights and future steps. Lancet Diabetes Endocrinol. 2022 Jul;10(7):475-476. doi: 10.1016/S2213-8587(22)00137-1.
- Starup-Linde J, Hygum K, Harslшf T, Langdahl B. Type 1 Diabetes and Bone Fragility: Links and Risks. Diabetes Metab Syndr Obes. 2019 Dec 3;12:2539-2547. doi: 10.2147/DMSO.S191091.
- Leslie WD, Rubin MR, Schwartz AV, Kanis JA. Type 2 diabetes and bone. J Bone Miner Res. 2012 Nov;27(11):2231-7. doi: 10.1002/jbmr.1759. Epub 2012 Sep 28. Erratum in: J Bone Miner Res. 2017 Nov;32(11):2319.
- De Araújo IM, Moreira MLM, de Paula FJA. Diabetes and bone. Arch Endocrinol Metab. 2022 Nov 11;66(5):633-641. doi: 10.20945/2359-3997000000552.
- Delitala AP, Scuteri A, Doria C. Thyroid Hormone Diseases and Osteoporosis. J Clin Med. 2020 Apr 6;9(4):1034. doi: 10.3390/jcm9041034.
- Arvind C, Ragul B, Sudha M. Prevalence of premenopausal osteoporosis in hypothyroid patients. Int J Adv Med. 2020;7(3):431-434. doi: 10.18203/2349-3933.ijam20200653.
- Lewandowski K, Kaniewska M, Więcek M, et al. Risk Factors for Osteoporosis among Patients with Inflammatory Bowel Disease-Do We Already Know Everything? Nutrients. 2023 Feb 24;15(5):1151. doi: 10.3390/nu15051151.
- van Bodegraven AA, Bravenboer N. Perspective on skeletal health in inflammatory bowel disease. Osteoporos Int. 2020 Apr;31(4):637-646. doi: 10.1007/s00198-019-05234-w.
- Rolvien T, Stürznickel J, Schmidt FN, et al. Comparison of Bone Microarchitecture Between Adult Osteogenesis Imperfecta and Early-Onset Osteoporosis. Calcif Tissue Int. 2018 Nov;103(5):512-521. doi: 10.1007/s00223-018-0447-8.
- Steinman J, Shibli-Rahhal A. Anorexia Nervosa and Osteoporosis: Pathophysiology and Treatment. J Bone Metab. 2019 Aug;26(3):133-143. doi: 10.11005/jbm.2019.26.3.133.
- Batteux B, Bennis Y, Bodeau S, et al. Associations between osteoporosis and drug exposure: A post-marketing study of the World Health Organization pharmacovigilance database (VigiBase®). Bone. 2021 Dec;153:116137. doi: 10.1016/j.bone.2021.116137.
- Mortensen SJ, Mohamadi A, Wright CL, et al. Medications as a Risk Factor for Fragility Hip Fractures: A Systematic Review and Meta-analysis. Calcif Tissue Int. 2020 Jul;107(1):1-9. doi: 10.1007/s00223-020-00688-1.
- Kanis JA, Johansson H, Oden A, et al. A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res. 2004 Jun;19(6):893-9. doi: 10.1359/JBMR.040134.
- Li L, Bensing S, Falhammar H. Rate of fracture in patients with glucocorticoid replacement therapy: a systematic review and meta-analysis. Endocrine. 2021 Oct;74(1):29-37. doi: 10.1007/s12020-021-02723-z.
- Loke YK, Gilbert D, Thavarajah M, Blanco P, Wilson AM. Bone mineral density and fracture risk with long-term use of inhaled corticosteroids in patients with asthma: systematic review and meta-analysis. BMJ Open. 2015 Nov 24;5(11):e008554. doi: 10.1136/bmjopen-2015-008554.
- Zhang YS, Zheng YD, Yuan Y, Chen SC, Xie BC. Effects of Anti-Diabetic Drugs on Fracture Risk: A Systematic Review and Network Meta-Analysis. Front Endocrinol (Lausanne). 2021 Oct 14;12:735824. doi: 10.3389/fendo.2021.735824.
- Ruanpeng D, Ungprasert P, Sangtian J, Harindhanavudhi T. Sodium-glucose cotransporter 2 (SGLT2) inhibitors and fracture risk in patients with type 2 diabetes mellitus: A meta-analysis. Diabetes Metab Res Rev. 2017 Sep;33(6). doi: 10.1002/dmrr.2903.
- Chai S, Liu F, Yang Z, et al. Risk of Fracture With Dipeptidyl Peptidase-4 Inhibitors, Glucagon-like Peptide-1 Receptor Agonists, or Sodium-Glucose Cotransporter-2 Inhibitors in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Network Meta-analysis Combining 177 Randomized Controlled Trials With a Median Follow-Up of 26 weeks. Front Pharmacol. 2022 Jul 1;13:825417. doi: 10.3389/fphar.2022.825417.
- Mercurio M, de Filippis R, Spina G, et al. The use of antidepressants is linked to bone loss: A systematic review and metanalysis. Orthop Rev (Pavia). 2022 Oct 13;14(6):38564. doi: 10.52965/001c.38564.
- Azimi Manavi B, Stuart AL, Pasco JA, et al. Use of antipsychotic medication and its relationship with bone mineral density: A population-based study of men and women. Front Psychiatry. 2023 Jan 5;13:1004366. doi: 10.3389/fpsyt.2022.1004366.
- Handa K, Kiyohara S, Yamakawa T, et al. Bone loss caused by dopaminergic degeneration and levodopa treatment in Parkinson's disease model mice. Sci Rep. 2019 Sep 24;9(1):13768. doi: 10.1038/s41598-019-50336-4.
- Köhler-Forsberg O, Rohde C, Nierenberg AA, Østergaard SD. Association of lithium treatment with the risk of osteoporosis in patients with bipolar disorder. JAMA Psychiatry. 2022 May 1;79(5):454-463. doi: 10.1001/jamapsychiatry.2022.0337.
- Poly TN, Islam MM, Yang HC, Li YJ. Association between benzodiazepines use and risk of hip fracture in the elderly people: A meta-analysis of observational studies. Joint Bone Spine. 2020 May;87(3):241-249. doi: 10.1016/j.jbspin.2019.11.003.
- da Maia TF, de Camargo BG, Pereira ME, de Oliveira CS, Guiloski IC. Increased Risk of Fractures and Use of Proton Pump Inhibitors in Menopausal Women: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022 Oct 19;19(20):13501. doi: 10.3390/ijerph192013501.
- Kanis JA, Johansson H, Harvey NC, McCloskey EV. A brief history of FRAX. Arch Osteoporos. 2018 Oct 31;13(1):118. doi: 10.1007/s11657-018-0510-0.
- Povoroznyuk V, Grуgorieva N, Kanis J, McCloskey E, Johansson H. Ukrainian Version of FRAX: from creation to validation. Pain, Joints, Spine. 2021;(3):5-14. doi: 10.22141/2224-1507.3.23.2016.85000.
- Povoroznyuk V, Grygorieva N, Johansson H, et al. FRAX-Based Intervention Thresholds for Osteoporosis Treatment in Ukraine. J Osteoporos. 2021 Jun 10;2021:2043479. doi: 10.1155/2021/2043479.
- Giangregorio LM, Leslie WD, Lix LM, et al. FRAX underestimates fracture risk in patients with diabetes. J Bone Miner Res. 2012 Feb;27(2):301-8. doi: 10.1002/jbmr.556.
- Grygorieva N, Musiienko A, Zaverukha N, Bystrytska M, Povoroznyuk R. Bone mineral density and probability of osteoporotic fractures in women with type ii diabetes mellitus. Wiad Lek. 2022;75(12):2920-2925. doi: 10.36740/WLek202212105.
- Mok CC, Tse SM, Chan KL, Ho LY. Estimation of fracture risk by the FRAX tool in patients with systemic lupus erythematosus: a 10-year longitudinal validation study. Ther Adv Musculoskelet Dis. 2022 Feb 9;14:1759720X221074451. doi: 10.1177/1759720X221074451.
- Kwok WS, Chung HY. Review Article on the Relationship between Spondyloarthritis and Osteoporosis. Journal of Clinical Rheumatology and Immunology. 2022;22(2):54-58. doi: 10.1142/S2661341722300117.
- Mok CC, Ho LY, Tse SM, et al. POS0171 Underestimation Of The Fracture Risk By The Frax Formula In Chronic Glucocorticoid Users: A 10-Year Longitudinal Validation Study. Annals of the Rheumatic Diseases 2021;80:298. doi: 10.1136/annrheumdis-2021-eular.3400.
- Kanis JA, Johansson H, Oden A, McCloskey EV. Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int. 2011 Mar;22(3):809-16. doi: 10.1007/s00198-010-1524-7.
- El Miedany Y. FRAX: re-adjust or re-think. Arch Osteoporos. 2020 Sep 28;15(1):150. doi: 10.1007/s11657-020-00827-z.
- Povoroznyuk VV, Grygorieva NV, Orlyk TV, Nyshkumai OI, Dzerovich NI, Balatskaya NI. Osteoporosis in the practice of an internist. Kyiv; 2014; 198 p.
- Povoroznyuk VV, Grygorіeva NV, Dedukh NV, eds. Secondary osteoporosis: a monograph. Kropyvnytskyi: Polium; 2021. 528 p.
- Schini M, Vilaca T, Gossiel F, Salam S, Eastell R. Bone Turnover Markers: Basic Biology to Clinical Applications. Endocr Rev. 2023 May 8;44(3):417-473. doi: 10.1210/endrev/bnac031.
- Fisher A, Fisher L, Srikusalanukul W, Smith PN. Bone Turnover Status: Classification Model and Clinical Implications. Int J Med Sci. 2018 Feb 1;15(4):323-338. doi: 10.7150/ijms.22747.
- Lorentzon M, Branco J, Brandi ML, et al. Algorithm for the Use of Biochemical Markers of Bone Turnover in the Diagnosis, Assessment and Follow-Up of Treatment for Osteoporosis. Adv Ther. 2019 Oct;36(10):2811-2824. doi: 10.1007/s12325-019-01063-9.
- Eastell R, Pigott T, Gossiel F, Naylor KE, Walsh JS, Peel NFA. Diagnosis of endocrine disease: Bone turnover markers: are they clinically useful? Eur J Endocrinol. 2018 Jan;178(1):R19-R31. doi: 10.1530/EJE-17-0585.
- Eastell R, Szulc P. Use of bone turnover markers in postmenopausal osteoporosis. Lancet Diabetes Endocrinol. 2017 Nov;5(11):908-923. doi: 10.1016/S2213-8587(17)30184-5.
- Johansson H, Odén A, Kanis JA, et al.; IFCC-IOF Joint Working Group on Standardisation of Biochemical Markers of Bone Turnover. A meta-analysis of reference markers of bone turnover for prediction of fracture. Calcif Tissue Int. 2014 May;94(5):560-7. doi: 10.1007/s00223-014-9842-y.
- Garnero P, Hausherr E, Chapuy MC, et al. Markers of bone resorption predict hip fracture in elderly women: the EPIDOS Prospective Study. J Bone Miner Res. 1996 Oct;11(10):1531-8. doi: 10.1002/jbmr.5650111021.
- Naylor KE, McCloskey EV, Jacques RM, et al. Clinical utility of bone turnover markers in monitoring the withdrawal of treatment with oral bisphosphonates in postmenopausal osteoporosis. Osteoporos Int. 2019 Apr;30(4):917-922. doi: 10.1007/s00198-018-04823-5.
- Hong L, Liu D, Wu F, Wang M, Cen Y, Ma L. Correlation between Bone Turnover Markers and Bone Mineral Density in Patients Undergoing Long-Term Anti-Osteoporosis Treatment: A Systematic Review and Meta-Analysis. Applied Sciences. 2020;10(3):832. doi: 10.3390/app10030832.
- Ivaska KK, Gerdhem P, Akesson K, Garnero P, Obrant KJ. Effect of fracture on bone turnover markers: a longitudinal study comparing marker levels before and after injury in 113 elderly women. J Bone Miner Res. 2007 Aug;22(8):1155-64. doi: 10.1359/jbmr.070505.
- Pan C, Liu X, Li T, Wang G, Sun J. Kinetic of bone turnover markers after osteoporotic vertebral compression fractures in postmenopausal female. J Orthop Surg Res. 2018 Dec 7;13(1):314. doi: 10.1186/s13018-018-1025-5.
- Johansson H, Odén A, Kanis JA et al.; IFCC-IOF Joint Working Group on Standardisation of Biochemical Markers of Bone Turnover. A meta-analysis of reference markers of bone turnover for prediction of fracture. Calcif Tissue Int. 2014 May;94(5):560-7. doi: 10.1007/s00223-014-9842-y.
- Silva BC, Leslie WD, Resch H et al. Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res. 2014 Mar;29(3):518-30. doi: 10.1002/jbmr.2176.
- Povorozniuk V, Dzerovych N, Hans D. Trabecular bone score in clinical practice (review). Orthopaedics traumatology and prosthetics. 2015;(2);126-136. doi: 10.15674/0030-598720152126-136.
- Kaloudis E-Th. Trabecular bone score for the evaluation of fracture risk: A literature review. JRPMS. 2022;6(4):121-127. doi: 10.22540/JRPMS-06-121.
- McCloskey EV, Odén A, Harvey NC, et al. A Meta-Analysis of Trabecular Bone Score in Fracture Risk Prediction and Its Relationship to FRAX. J Bone Miner Res. 2016 May;31(5):940-8. doi: 10.1002/jbmr.2734.
- Grygorieva NV, Zubach OB. Peculiarities of the geometry of the proximal part of the femur as an independent risk factor for its fractures (literature review). Problems of osteology. 2015;18(4):3-11.
- Grygorieva NV, Povoroznyuk VV, Povoroznyuk VasV, Zubach OB. Reference indices of hip structural analysis in Ukrainian women. Pain, Joints, Spine. 2017;7(4):152-160. doi: 10.22141/2224-1507.7.4.2017.121226.
- Marín F, González-Macías J, Díez-Pérez A, Palma S, Delgado-Rodríguez M. Relationship between bone quantitative ultrasound and fractures: a meta-analysis. J Bone Miner Res. 2006 Jul;21(7):1126-35. doi: 10.1359/jbmr.060417.
- Moayyeri A, Adams JE, Adler RA, et al. Quantitative ultrasound of the heel and fracture risk assessment: an updated meta-analysis. Osteoporos Int. 2012 Jan;23(1):143-53. doi: 10.1007/s00198-011-1817-5.
- McCloskey EV, Kanis JA, Odén A, et al. Predictive ability of heel quantitative ultrasound for incident fractures: an individual-level meta-analysis. Osteoporos Int. 2015 Jul;26(7):1979-87. doi: 10.1007/s00198-015-3072-7.
- Escobio-Prieto I, Blanco-Díaz M, Pinero-Pinto E, Rodriguez-Rodriguez AM, Ruiz-Dorantes FJ, Albornoz-Cabello M. Quantitative Ultrasound and Bone Health in Elderly People, a Systematic Review. Biomedicines. 2023 Apr 13;11(4):1175. doi: 10.3390/biomedicines11041175.
- Mortensen SJ, Beeram I, Florance J, et al. Modifiable lifestyle factors associated with fragility hip fracture: a systematic review and meta-analysis. J Bone Miner Metab. 2021 Sep;39(5):893-902. doi: 10.1007/s00774-021-01230-5.
- Clemson L, Stark S, Pighills AC, et al. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2023 Mar 10;3(3):CD013258. doi: 10.1002/14651858.CD013258.pub2.
- Grygorieva N, Dedukh N, Parubets M, Bystrytska M. Disuse (post-immobilization) osteoporosis: literature review and clinical case series. Pain, Joints, Spine. 2022;12(3):94–107. doi: 10.22141/pjs.12.3.2022.335.
- Kast S, Shojaa M, Kohl M, et al. Effects of different exercise intensity on bone mineral density in adults: a comparative systematic review and meta-analysis. Osteoporos Int. 2022 Aug;33(8):1643-1657. doi: 10.1007/s00198-022-06329-7.
- Shojaa M, von Stengel S, Kohl M, Schoene D, Kemmler W. Effects of dynamic resistance exercise on bone mineral density in postmenopausal women: a systematic review and meta-analysis with special emphasis on exercise parameters. Osteoporos Int. 2020 Aug;31(8):1427-1444. doi: 10.1007/s00198-020-05441-w.
- Schinzel E, Kast S, Kohl M, et al. The effect of aquatic exercise on bone mineral density in older adults. A systematic review and meta-analysis. Front Physiol. 2023 Mar 13;14:1135663. doi: 10.3389/fphys.2023.1135663.
- Sanchez-Trigo H, Rittweger J, Saсudo B. Effects of non-supervised exercise interventions on bone mineral density in adult women: a systematic review and meta‑analysis. Osteoporos Int. 2022 Jul;33(7):1415-1427. doi: 10.1007/s00198-022-06357-3.
- Howe TE, Shea B, Dawson LJ, et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev. 2011 Jul 6;(7):CD000333. doi: 10.1002/14651858.CD000333.pub2.
- Kemmler W, Häberle L, von Stengel S. Effects of exercise on fracture reduction in older adults: a systematic review and meta-analysis. Osteoporos Int. 2013 Jul;24(7):1937-50. doi: 10.1007/s00198-012-2248-7.
- Hoffmann I, Kohl M, von Stengel S, et al. Exercise and the prevention of major osteoporotic fractures in adults: a systematic review and meta-analysis with special emphasis on intensity progression and study duration. Osteoporos Int. 2023 Jan;34(1):15-28. doi: 10.1007/s00198-022-06592-8.
- Hoffmann I, Shojaa M, Kohl M, et al. Exercise Reduces the Number of Overall and Major Osteoporotic Fractures in Adults. Does Supervision Make a Difference? Systematic Review and Meta-Analysis. J Bone Miner Res. 2022 Nov;37(11):2132-2148. doi: 10.1002/jbmr.4683.
- Gibbs JC, MacIntyre NJ, Ponzano M, et al. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev. 2019 Jul 5;7(7):CD008618. doi: 10.1002/14651858.CD008618.pub3.
- Pantouvaki A, Patelarou E, Kastanis G, Alpantaki K, Sfakianakis MZ. The effect of an exercise-based rehabilitation programme in functional recovery and prevention of secondary falls after a hip fracture in older adults: A systematic review. J Frailty Sarcopenia Falls. 2023 Jun 1;8(2):118-126. doi: 10.22540/JFSF-08-118.
- Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019 Jan 31;1(1):CD012424. doi: 10.1002/14651858.CD012424.pub2.
- El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013 Oct 29;347:f6234. doi: 10.1136/bmj.f6234.
- Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 Sep 12;2012(9):CD007146. doi: 10.1002/14651858.CD007146.pub3.
- Lomas-Vega R, Obrero-Gaitбn E, Molina-Ortega FJ, Del-Pino-Casado R. Tai Chi for Risk of Falls. A Meta-analysis. J Am Geriatr Soc. 2017 Sep;65(9):2037-2043. doi: 10.1111/jgs.15008.
- Huang ZG, Feng YH, Li YH, Lv CS. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open. 2017 Feb 6;7(2):e013661. doi: 10.1136/bmjopen-2016-013661.
- Alin CK, Frisendahl N, Kronhed AG, Salminen H. Experiences of using an activating spinal orthosis in women with osteoporosis and back pain in primary care. Arch Osteoporos. 2020 Oct 29;15(1):171. doi: 10.1007/s11657-020-00754-z.
- Kaijser Alin C, Uzunel E, Grahn Kronhed AC, Alinaghizadeh H, Salminen H. Effect of treatment on back pain and back extensor strength with a spinal orthosis in older women with osteoporosis: a randomized controlled trial. Arch Osteoporos. 2019 Jan 9;14(1):5. doi: 10.1007/s11657-018-0555-0.
- Jacobs E, Senden R, McCrum C, van Rhijn LW, Meijer K, Willems PC. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin Interv Aging. 2019 Apr 11;14:671-680. doi: 10.2147/CIA.S199853.
- Sánchez-Pinto-Pinto B, Romero-Morales C, López-López D, de-Labra C, García-Pérez-de-Sevilla G. Efficacy of Bracing on Thoracic Kyphotic Angle and Functionality in Women with Osteoporosis: A Systematic Review. Medicina (Kaunas). 2022 May 24;58(6):693. doi: 10.3390/medicina58060693.
- Kweh BTS, Lee HQ, Tan T, et al. Role of Spinal Orthoses in Osteoporotic Vertebral Fractures of the Elderly Population (Age 60 Years or Older): Systematic Review. Global Spine J. 2021 Jul;11(6):975-987. doi: 10.1177/2192568220948036.
- Pieroh P, Spiegl UJA, Völker A, et al.; Spine Section of the German Society for Orthopaedics and Trauma. Spinal Orthoses in the Treatment of Osteoporotic Thoracolumbar Vertebral Fractures in the Elderly: A Systematic Review With Quantitative Quality Assessment. Global Spine J. 2023 Apr;13(1_suppl):59S-72S. doi: 10.1177/21925682221130048.
- Jin YZ, Lee JH. Effect of Brace to Osteoporotic Vertebral Fracture: a Meta-Analysis. J Korean Med Sci. 2016 Oct;31(10):1641-9. doi: 10.3346/jkms.2016.31.10.1641.
- Furrer PR, Hodel S, Wanivenhaus F, Grubhofer F, Farshad M. Compliance with wearing a thoracolumbar orthosis in nonoperative treatment of osteoporotic vertebral fractures: a prospective sensor-controlled study. Spine J. 2023 Mar;23(3):433-439. doi: 10.1016/j.spinee.2022.11.009.
- Santesso N, Carrasco-Labra A, Brignardello-Petersen R. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev. 2014 Mar 31;(3):CD001255. doi: 10.1002/14651858.CD001255.pub5.
- Webster J, Rycroft CE, Greenwood DC, Cade JE. Dietary risk factors for hip fracture in adults: An umbrella review of meta-analyses of prospective cohort studies. PLoS One. 2021 Nov 10;16(11):e0259144. doi: 10.1371/journal.pone.0259144.
- Order of the Ministry of Health of Ukraine No 1073 dated September 3, 2017. On the approval of the norms of physiological needs of the population of Ukraine in basic food substances and energy. Available from: https://zakon.rada.gov.ua/laws/show/z1206-17#Text. Accessed: 2023 31 Aug.
- Grygorieva N, Povoroznyuk V, Romanenko M, Synieok L. Calcium intake in an adult Ukrainian population. Arch Osteoporos. 2020 Feb 23;15(1):23. doi: 10.1007/s11657-020-0712-0.
- Grygorieva N, Solonenko T, Musiienko A. Vitamin D deficiency during the COVID-19 pandemic and war in Ukraine. Pain, Joints, Spine. 2023;13(1);7-14. doi: 10.22141/pjs.13.1.2023.352.
- Grygorieva N, Tronko M, Kovalenko V, et al. Diagnosis, prevention and treatment of vitamin D deficiency in adults: Ukrainian experts consensus statement. Pain, Joints, Spine. 2023;13(2):60-76. doi: 10.22141/pjs.13.2.2023.368.
- Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ. 2015 Sep 29;351:h4183. doi: 10.1136/bmj.h4183.
- Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ. 2015 Sep 29;351:h4580. doi: 10.1136/bmj.h4580.
- Bolland MJ, Grey A, Avenell A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 2018 Nov;6(11):847-858. doi: 10.1016/S2213-8587(18)30265-1.
- Kong SH, Jang HN, Kim JH, Kim SW, Shin CS. Effect of Vitamin D Supplementation on Risk of Fractures and Falls According to Dosage and Interval: A Meta-Analysis. Endocrinol Metab (Seoul). 2022 Apr;37(2):344-358. doi: 10.3803/EnM.2021.1374.
- Thanapluetiwong S, Chewcharat A, Takkavatakarn K, Praditpornsilpa K, Eiam-Ong S, Susantitaphong P. Vitamin D supplement on prevention of fall and fracture: A Meta-analysis of Randomized Controlled Trials. Medicine (Baltimore). 2020 Aug 21;99(34):e21506. doi: 10.1097/MD.0000000000021506.
- Yao P, Bennett D, Mafham M, et al. Vitamin D and Calcium for the Prevention of Fracture: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019 Dec 2;2(12):e1917789. doi: 10.1001/jamanetworkopen.2019.17789.
- Zhao JG, Zeng XT, Wang J, Liu L. Association Between Calcium or Vitamin D Supplementation and Fracture Incidence in Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. JAMA. 2017 Dec 26;318(24):2466-2482. doi: 10.1001/jama.2017.19344.
- Avenell A, Mak JC, O'Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev. 2014 Apr 14;2014(4):CD000227. doi: 10.1002/14651858.CD000227.pub4.
- Weaver CM, Alexander DD, Boushey CJ, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016 Jan;27(1):367-76. doi: 10.1007/s00198-015-3386-5. Epub 2015 Oct 28. Erratum in: Osteoporos Int. 2016 Aug;27(8):2643-6.
- Liu C, Kuang X, Li K, Guo X, Deng Q, Li D. Effects of combined calcium and vitamin D supplementation on osteoporosis in postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. Food Funct. 2020 Dec 1;11(12):10817-10827. doi: 10.1039/d0fo00787k.
- Carmel AS, Shieh A, Bang H, Bockman RS. The 25(OH)D level needed to maintain a favorable bisphosphonate response is ≥33 ng/ml. Osteoporos Int. 2012 Oct;23(10):2479-87. doi: 10.1007/s00198-011-1868-7.
- Sugimoto T, Matsumoto T, Hosoi T, et al. Efficacy of denosumab co-administered with vitamin D and Ca by baseline vitamin D status. J Bone Miner Metab. 2020 Nov;38(6):848-858. doi: 10.1007/s00774-020-01119-9.
- Suzuki T, Nakamura Y, Kato H. Calcium and vitamin D supplementation with 3-year denosumab treatment is beneficial to enhance bone mineral density in postmenopausal patients with osteoporosis and rheumatoid arthritis. Ther Clin Risk Manag. 2018 Dec 18;15:15-22. doi: 10.2147/TCRM.S182858.
- Lu K, Shi Q, Gong YQ, Li C. Association between vitamin D and zoledronate-induced acute-phase response fever risk in osteoporotic patients. Front Endocrinol (Lausanne). 2022 Oct 10;13:991913. doi: 10.3389/fendo.2022.991913.
- Shams-White MM, Chung M, Du M, et al. Dietary protein and bone health: a systematic review and meta-analysis from the National Osteoporosis Foundation. Am J Clin Nutr. 2017 Jun;105(6):1528-1543. doi: 10.3945/ajcn.116.145110.
- Wu AM, Sun XL, Lv QB, et al. The relationship between dietary protein consumption and risk of fracture: a subgroup and dose-response meta-analysis of prospective cohort studies. Sci Rep. 2015 Mar 16;5:9151. doi: 10.1038/srep09151.
- Wallace TC, Frankenfeld CL. Dietary Protein Intake above the Current RDA and Bone Health: A Systematic Review and Meta-Analysis. J Am Coll Nutr. 2017 Aug;36(6):481-496. doi: 10.1080/07315724.2017.1322924.
- Rizzoli R, Biver E, Bonjour JP, et al. Benefits and safety of dietary protein for bone health-an expert consensus paper endorsed by the European Society for Clinical and Economical Aspects of Osteopororosis, Osteoarthritis, and Musculoskeletal Diseases and by the International Osteoporosis Foundation. Osteoporos Int. 2018 Sep;29(9):1933-1948. doi: 10.1007/s00198-018-4534-5.
- Amin U, McPartland A, O'Sullivan M, Silke C. An overview of the management of osteoporosis in the aging female population. Womens Health (Lond). 2023 Jan-Dec;19:17455057231176655. doi: 10.1177/17455057231176655.
- Rogers MJ, Mönkkönen J, Munoz MA. Molecular mechanisms of action of bisphosphonates and new insights into their effects outside the skeleton. Bone. 2020 Oct;139:115493. doi: 10.1016/j.bone.2020.115493.
- Compston J. Practical guidance for the use of bisphosphonates in osteoporosis. Bone. 2020 Jul;136:115330. doi: 10.1016/j.bone.2020.115330.
- Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD001155. doi: 10.1002/14651858.CD001155.pub2.
- Wells G, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD004523. doi: 10.1002/14651858.CD004523.pub3.
- Delmas PD, Recker RR, Chesnut CH 3rd, et al. Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int. 2004 Oct;15(10):792-8. doi: 10.1007/s00198-004-1602-9.
- Chesnut CH 3rd, Skag A, Christiansen C, et al.; Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE). Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004 Aug;19(8):1241-9. doi: 10.1359/JBMR.040325.
- Inderjeeth C, Glendenning P, Ratnagobal S, Inderjeeth D, Ondhia C. Long-term efficacy, safety, and patient acceptability of ibandronate in the treatment of postmenopausal osteoporosis. Int J Womens Health. 2015;7:7-17. doi: 10.2147/IJWH.S73944.
- Nakamura T, Ito M, Hashimoto J, et al.; MOVEST Study Group. Clinical efficacy and safety of monthly oral ibandronate 100 mg versus monthly intravenous ibandronate 1 mg in Japanese patients with primary osteoporosis. Osteoporos Int. 2015 Nov;26(11):2685-93. doi: 10.1007/s00198-015-3175-1.
- Paggiosi MA, Peel N, McCloskey E, Walsh JS, Eastell R. Comparison of the effects of three oral bisphosphonate therapies on the peripheral skeleton in postmenopausal osteoporosis: the TRIO study. Osteoporos Int. 2014 Dec;25(12):2729-41. doi: 10.1007/s00198-014-2817-z.
- Black DM, Delmas PD, Eastell R, et al.; HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007 May 3;356(18):1809-22. doi: 10.1056/NEJMoa067312.
- Lyles KW, Colуn-Emeric CS, Magaziner JS, et al.; HORIZON Recurrent Fracture Trial. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007 Nov 1;357(18):1799-809. doi: 10.1056/NEJMoa074941.
- Singh M, Gonegandla GS. Bisphosphonate-Induced Osteonecrosis of the Jaws (BIONJ). J Maxillofac Oral Surg. 2020 Jun;19(2):162-167. doi: 10.1007/s12663-019-01211-2.
- Khan AA, Morrison A, Hanley DA, et al.; International Task Force on Osteonecrosis of the Jaw. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res. 2015 Jan;30(1):3-23. doi: 10.1002/jbmr.2405.
- Larsen MS, Schmal H. The enigma of atypical femoral fractures: A summary of current knowledge. EFORT Open Rev. 2018 Sep 12;3(9):494-500. doi: 10.1302/2058-5241.3.170070.
- Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014 Jan;29(1):1-23. doi: 10.1002/jbmr.1998.
- Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res. 2013 Aug;28(8):1729-37. doi: 10.1002/jbmr.1893.
- Beth-Tasdogan NH, Mayer B, Hussein H, Zolk O, Peter JU. Interventions for managing medication-related osteonecrosis of the jaw. Cochrane Database Syst Rev. 2022 Jul 12;7(7):CD012432. doi: 10.1002/14651858.CD012432.pub3. PMID: 35866376; PMCID: PMC9309005.
- Cummings SR, San Martin J, McClung MR, et al.; FREEDOM Trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009 Aug 20;361(8):756-65. doi: 10.1056/NEJMoa0809493. Epub 2009 Aug 11. Erratum in: N Engl J Med. 2009 Nov 5;361(19):1914.
- Bone HG, Wagman RB, Brandi ML, et al. 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol. 2017 Jul;5(7):513-523. doi: 10.1016/S2213-8587(17)30138-9.
- Cosman F, Huang S, McDermott M, Cummings SR. Multiple Vertebral Fractures After Denosumab Discontinuation: FREEDOM and FREEDOM Extension Trials Additional Post Hoc Analyses. J Bone Miner Res. 2022 Nov;37(11):2112-2120. doi: 10.1002/jbmr.4705.
- Chapurlat R. Effects and management of denosumab discontinuation. Joint Bone Spine. 2018 Oct;85(5):515-517. doi: 10.1016/j.jbspin.2017.12.013.
- Guaсabens N, Moro-Бlvarez MJ, Casado E, et al.; SEIOMM Working Group. The next step after anti-osteoporotic drug discontinuation: an up-to-date review of sequential treatment. Endocrine. 2019 Jun;64(3):441-455. doi: 10.1007/s12020-019-01919-8.
- De Villiers TJ, Tatarchuk TF, Avramenko NV et al. National consensus on the management of menopausal patients. Reproductive endocrinology. 2016;1(27):8-25. doi: 10.18370/2309-4117.2016.27.8-25.
- Tatarchuk TF, Anikusko MF, Bulavenko OV and others. Clinical guideline based on evidence: Menopausal disorders and other disorders in the perimenopausal period. 2022. Available from: https://repo.dma.dp.ua/7804. Accessed: 2023 30 Aug.
- Marjoribanks J, Farquhar C, Roberts H, Lethaby A, Lee J. Long-term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst Rev. 2017 Jan 17;1(1):CD004143. doi: 10.1002/14651858.CD004143.pub5.
- Stepan JJ, Hruskova H, Kverka M. Update on Menopausal Hormone Therapy for Fracture Prevention. Curr Osteoporos Rep. 2019 Dec;17(6):465-473. doi: 10.1007/s11914-019-00549-3.
- Zhang GQ, Chen JL, Luo Y, et al. Menopausal hormone therapy and women's health: An umbrella review. PLoS Med. 2021 Aug 2;18(8):e1003731. doi: 10.1371/journal.pmed.1003731.
- Torgerson DJ, Bell-Syer SE. Hormone replacement therapy and prevention of vertebral fractures: a meta-analysis of randomised trials. BMC Musculoskelet Disord. 2001;2:7. doi: 10.1186/1471-2474-2-7.
- Torgerson DJ, Bell-Syer SE. Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials. JAMA. 2001 Jun 13;285(22):2891-7. doi: 10.1001/jama.285.22.2891.
- Zhu Linlin, Jiang Xinyan MS, Sun Yuhong, Shu Wenhuan. Effect of hormone therapy on the risk of bone fractures: a systematic review and meta-analysis of randomized controlled trials. Menopause 23(4):p 461-470, April 2016. doi: 10.1097/GME.0000000000000519.
- Greenspan SL, Resnick NM, Parker RA. Combination therapy with hormone replacement and alendronate for prevention of bone loss in elderly women: a randomized controlled trial. JAMA. 2003 May 21;289(19):2525-33. doi: 10.1001/jama.289.19.2525.
- Barrett-Connor E, Wehren LE, Siris ES, et al. Recency and duration of postmenopausal hormone therapy: effects on bone mineral density and fracture risk in the National Osteoporosis Risk Assessment (NORA) study. Menopause. 2003 Sep-Oct;10(5):412-9. doi: 10.1097/01.GME.0000086467.82759.DA.
- Cauley JA, Robbins J, Chen Z, et al.; Women's Health Initiative Investigators. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women's Health Initiative randomized trial. JAMA. 2003 Oct 1;290(13):1729-38. doi: 10.1001/jama.290.13.1729.
- Effects of hormone therapy on bone mineral density: results from the postmenopausal estrogen/progestin interventions (PEPI) trial. The Writing Group for the PEPI. JAMA. 1996 Nov 6;276(17):1389-96.
- Kloosterboer HJ. Tissue-selectivity: the mechanism of action of tibolone. Maturitas. 2004 Aug 30;48 Suppl. 1:S30-40. doi: 10.1016/j.maturitas.2004.02.012.
- Castrejón-Delgado L, Castelán-Martínez OD, Clark P, Garduño-Espinosa J, Mendoza-Núñez VM, Sánchez-Rodríguez MA. Effect of Tibolone on Bone Mineral Density in Postmenopausal Women: Systematic Review and Meta-Analysis. Biology (Basel). 2021 Mar 10;10(3):211. doi: 10.3390/biology10030211.
- Cummings SR, Ettinger B, Delmas PD, et al.; LIFT Trial Investigators. The effects of tibolone in older postmenopausal women. N Engl J Med. 2008 Aug 14;359(7):697-708. doi: 10.1056/NEJMoa0800743.
- Formoso G, Perrone E, Maltoni S, et al. Short and long term effects of tibolone in postmenopausal women. Cochrane Database Syst Rev. 2012 Feb 15;(2):CD008536. doi: 10.1002/14651858.CD008536.pub2. Update in: Cochrane Database Syst Rev. 2016 Oct 12;10 :CD008536.
- Barrionuevo P, Kapoor E, Asi N, et al. Efficacy of Pharmacological Therapies for the Prevention of Fractures in Postmenopausal Women: A Network Meta-Analysis. J Clin Endocrinol Metab. 2019 May 1;104(5):1623-1630. doi: 10.1210/jc.2019-00192.
- Moshi MR, Nicolopoulos K, Stringer D, Ma N, Jenal M, Vreugdenburg T. The Clinical Effectiveness of Denosumab (Prolia®) for the Treatment of Osteoporosis in Postmenopausal Women, Compared to Bisphosphonates, Selective Estrogen Receptor Modulators (SERM), and Placebo: A Systematic Review and Network Meta-Analysis. Calcif Tissue Int. 2023 Jun;112(6):631-646. doi: 10.1007/s00223-023-01078-z.
- Davis S, Simpson E, Hamilton J, et al. Denosumab, raloxifene, romosozumab and teriparatide to prevent osteoporotic fragility fractures: a systematic review and economic evaluation. Health Technol Assess. 2020 Jun;24(29):1-314. doi: 10.3310/hta24290.
- Stevenson M, Jones ML, De Nigris E, Brewer N, Davis S, Oakley J. A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Health Technol Assess. 2005 Jun;9(22):1-160. doi: 10.3310/hta9220.
- Albert SG, Reddy S. Clinical evaluation of cost efficacy of drugs for treatment of osteoporosis: a meta-analysis. Endocr Pract. 2017 Jul;23(7):841-856. doi: 10.4158/EP161678.RA.
- Tan EH, Robinson DE, Jödicke AM, et al. Drug utilization analysis of osteoporosis medications in seven European electronic health databases. Osteoporos Int. 2023 Jul 12. doi: 10.1007/s00198-023-06837-0. Epub ahead of print.
- Compston JE, Drake MT. Defining Very High Fracture Risk: Is FRAX Fit for Purpose? J Bone Miner Res. 2020 Aug;35(8):1399-1403. doi: 10.1002/jbmr.4134.
- Kanis JA, Harvey NC, McCloskey E, et al. Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int. 2020 Jan;31(1):1-12. doi: 10.1007/s00198-019-05176-3.
- Curtis EM, Reginster JY, Al-Daghri N, et al. Management of patients at very high risk of osteoporotic fractures through sequential treatments. Aging Clin Exp Res. 2022 Apr;34(4):695-714. doi: 10.1007/s40520-022-02100-4.
- National Osteoporosis Guideline Group-UK. NOGG 2021: Clinical guideline for the prevention and treatment of osteoporosis. Available from: https://www.nogg.org.uk/full-guideline. Accessed: 2023, 31 Aug.
- Kanis JA, Johansson H, Harvey NC, et al. An assessment of intervention thresholds for very high fracture risk applied to the NOGG guidelines: A report for the National Osteoporosis Guideline Group (NOGG). Osteoporos Int. 2021 Oct;32(10):1951-1960. doi: 10.1007/s00198-021-05942-2.
- Ferrari S, Lippuner K, Lamy O, Meier C. 2020 recommendations for osteoporosis treatment according to fracture risk from the Swiss Association against Osteoporosis (SVGO). Swiss Med Wkly. 2020 Sep 29;150:w20352. doi: 10.4414/smw.2020.20352.
- Gregson CL, Armstrong DJ, Bowden J, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2022 Apr 5;17(1):58. doi: 10.1007/s11657-022-01061-5. Erratum in: Arch Osteoporos. 2022 May 19;17(1):80.
- Scottish Intercollegiate Guidelines Network (SIGN). Management of osteoporosis and the prevention of fragility fractures. Edinburgh: SIGN; 2021. (SIGN publication no. 142). Available from: https://www.sign.ac.uk/our-guidelines/management-of-osteoporosis-and-the-prevention-of-fragility-fractures. Accessed: 2023, 30 Aug.
- Shoback D, Rosen CJ, Black DM, Cheung AM, Murad MH, Eastell R. Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Guideline Update. J Clin Endocrinol Metab. 2020 Mar 1;105(3):dgaa048. doi: 10.1210/clinem/dgaa048.
- Cooper C, Javaid K, Elliot M et al. UK consensus guideline on the management of patients at low, high, and very high risk of osteoporotic fracture. Guidelines, 2020. Available from: https://www.medscape.co.uk/viewarticle/osteoporosis-assessing-and-managing-patients-low-high-and-2022a10017c9. Accessed: 2023, 30 Aug.
- Cosman F, Crittenden DB, Ferrari S, et al. FRAME Study: The Foundation Effect of Building Bone With 1 Year of Romosozumab Leads to Continued Lower Fracture Risk After Transition to Denosumab. J Bone Miner Res. 2018 Jul;33(7):1219-1226. doi: 10.1002/jbmr.3427.
- Saag KG, Petersen J, Brandi ML, et al. Romosozumab or Alendronate for Fracture Prevention in Women with Osteoporosis. N Engl J Med. 2017 Oct 12;377(15):1417-1427. doi: 10.1056/NEJMoa1708322.
- Kendler DL, Marin F, Zerbini CAF, et al. Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet. 2018 Jan 20;391(10117):230-240. doi: 10.1016/S0140-6736(17)32137-2.
- Foessl I, Dimai HP, Obermayer-Pietsch B. Long-term and sequential treatment for osteoporosis. Nat Rev Endocrinol. 2023 Jul 18. doi: 10.1038/s41574-023-00866-9. Epub ahead of print.
- Adler RA, El-Hajj Fuleihan G, et al. Managing Osteoporosis in Patients on Long-Term Bisphosphonate Treatment: Report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2016 Jan;31(1):16-35. doi: 10.1002/jbmr.2708.
- Meier C, Uebelhart B, Aubry-Rozier B, et al. Osteoporosis drug treatment: duration and management after discontinuation. A position statement from the SVGO/ASCO. Swiss Med Wkly. 2017 Aug 16;147:w14484. doi: 10.4414/smw.2017.14484.
- Díez-Pérez A, González-Macías J. Inadequate responders to osteoporosis treatment: proposal for an operational definition. Osteoporos Int. 2008 Nov;19(11):1511-6. doi: 10.1007/s00198-008-0659-2.
- BlackDM, Schwartz AV, Ensrud KE, et al; FLEX Research Group. Effects of continuing or stopping alendronate after 5 years of treatment: the fracture intervention trial long-term extension (FLEX): a randomized trial. JAMA. 2006 Dec 27;296(24):2927-38. doi: 10.1001/jama.296.24.2927.
- Ensrud KE, Barrett-Connor EL, Schwartz A, et al, Fracture Intervention Trial Long-Term Extension Research Group.Randomized trial of effect of alendronate continuation versus discontinuation in women with low BMD: results from the fracture intervention trial long-term extension. J Bone Miner Res. 2004 Aug;19(8):1259-69. doi: 10.1359/JBMR.040326.
- Watts NB, Chines A, Olszynski WP, et al. Fracture risk remains reduced one year after discontinuation of risedronate. Osteoporos Int. 2008 Mar;19(3):365-72. doi: 10.1007/s00198-007-0460-7.
- Eastell R, Hannon RA, Wenderoth D, Rodriguez-Moreno J, Sawicki A. Effect of stopping risedronate after long-term treatment on bone turnover. J Clin Endocrinol Metab. 2011 Nov;96(11):3367-73. doi: 10.1210/jc.2011-0412.
- Ravn P, Christensen JO, Baumann M, Clemmesen B. Changes in biochemical markers and bone mass after withdrawal of ibandronate treatment: prediction of bone mass changes during treatment. Bone. 1998 May;22(5):559-64. doi: 10.1016/s8756-3282(98)00044-1.
- Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012 Feb;27(2):243-54. doi: 10.1002/jbmr.1494.
- Tay WL, Tay D. Discontinuing Denosumab: Can It Be Done Safely? A Review of the Literature. Endocrinol Metab (Seoul). 2022 Apr;37(2):183-194. doi: 10.3803/EnM.2021.1369.
- Reid IR, Horne AM, Mihov B, Gamble GD. Bone Loss After Denosumab: Only Partial Protection with Zoledronate. Calcif Tissue Int. 2017 Oct;101(4):371-374. doi: 10.1007/s00223-017-0288-x.
- Kondo H, Okimoto N, Yoshioka T, et al. Zoledronic acid sequential therapy could avoid disadvantages due to the discontinuation of less than 3-year denosumab treatment. J Bone Miner Metab. 2020 Nov;38(6):894-902. doi: 10.1007/s00774-020-01126-w.
- Sølling AS, Tsourdi E, Harsløf T, Langdahl BL. Denosumab Discontinuation. Curr Osteoporos Rep. 2023 Feb;21(1):95-103. doi: 10.1007/s11914-022-00771-6.
- Chandran M. The why and how of sequential and combination therapy in osteoporosis. A review of the current evidence. Arch Endocrinol Metab. 2022 Nov 11;66(5):724-738. doi: 10.20945/2359-3997000000564.
- Kalashnikov A, Lazarenko Y, Kalashnikov O. Proximal Femoral Fractures: Structure, Factors of Occurrence, and Treatment Principles (Literature Review). Terra Orthopaedica, 2022;2(113):80-85. doi: 10.37647/0132-2486-2022-113-2-80-85.
- Zubach O, Grygorieva N, Povoroznyuk V. 10-year mortality in patients after hip fractures. Georgian Med News. 2021 Jan;(310):19-23. Russian.
- Kalashnikov A, Lazarenko Y, Kalashnikov O. Proximal femoral fractures: social significance and surgical treatment (review). Trauma. 2023;24(1):79-85. doi: 10.22141/1608-1706.1.24.2023.936.
- Tang X, Wang D, Liu Y, et al. The comparison between total hip arthroplasty and hemiarthroplasty in patients with femoral neck fractures: a systematic review and meta-analysis based on 25 randomized controlled trials. J Orthop Surg Res. 2020 Dec 10;15(1):596. doi: 10.1186/s13018-020-02122-6.
- Shan L, Shan B, Graham D, Saxena A. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthritis Cartilage. 2014 Mar;22(3):389-406. doi: 10.1016/j.joca.2013.12.006.
- Li X, Luo J. Hemiarthroplasty compared to total hip arthroplasty for the treatment of femoral neck fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2021 Mar 3;16(1):172. doi: 10.1186/s13018-020-02186-4.
- Buchbinder R, Johnston RV, Rischin KJ, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev. 2018 Nov 6;11(11):CD006349. doi: 10.1002/14651858.CD006349.pub4.
- Lou S, Shi X, Zhang X, Lyu H, Li Z, Wang Y. Percutaneous vertebroplasty versus non-operative treatment for osteoporotic vertebral compression fractures: a meta-analysis of randomized controlled trials. Osteoporos Int. 2019 Dec;30(12):2369-2380. doi: 10.1007/s00198-019-05101-8.
- Clark W, Diamond T. Early Vertebroplasty for Severely Painful Acute Osteoporotic Compression Fractures: A Critical Review of the Literature. Cardiovasc Intervent Radiol. 2023 Jan 18. doi: 10.1007/s00270-022-03348-z.
- Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016 Oct 1;388(10052):1408-1416. doi: 10.1016/S0140-6736(16)31341-1.
- Zhu RS, Kan SL, Ning GZ, et al. Which is the best treatment of osteoporotic vertebral compression fractures: balloon kyphoplasty, percutaneous vertebroplasty, or non-surgical treatment? A Bayesian network meta-analysis. Osteoporos Int. 2019 Feb;30(2):287-298. doi: 10.1007/s00198-018-4804-2.