Журнал «Здоровье ребенка» 1 (60) 2015
Вернуться к номеру
Asthenia in Children with Chronic Viral Hepatitis
Авторы: Lembryk I.S. — State Higher Educational Institution «Ivano-Frankivsk National Medical University»,
Department of Pediatrics, Ivano-Frankivsk, Ukraine
Рубрики: Педиатрия/Неонатология
Разделы: Клинические исследования
Версия для печати
In the article results of own researches concerning peculiarities of the course of asthenic syndrome in school-aged children with chronic hepatitis B, C and mixed forms are provided. It is established that chronic hepatitis C as well as a mixed hepatitis are accompanied by more evident symptoms of deadaptation and somatogenic asthenia than hepatitis B in which psychogenic manifestations prevailed. The degree of endogenous intoxication was also higher at hepatitis C.
У статті наведені результати власних спостережень стосовно особливостей перебігу астенічного синдрому в дітей шкільного віку, хворих на хронічний вірусний гепатит В, С і мікст-форми. Установлено, що хронічний гепатит С, а також мікст-гепатит супроводжуються більш вираженими симптомами дезадаптації і соматогенної астенії, аніж гепатит В, при якому превалювали психогенні прояви. Рівень ендогенної інтоксикації також був вищим при гепатиті С.
В статье приведены результаты собственных наблюдений касательно особенностей течения астенического синдрома у детей школьного возраста, больных хроническим гепатитом В, С и микст-формами. Установлено, что хронический гепатит С, а также микст-гепатит сопровождаются более выраженными симптомами дезадаптации и соматогенной астении, чем гепатит В, при котором превалировали психогенные проявления. Уровень эндогенной интоксикации также был выше при гепатите С.
children, asthenia, adaptation, hepatitis.
діти, астенія, адаптація, гепатит.
дети, астения, адаптация, гепатит.
Статья опубликована на с. 25-28
Introduction
At least 360 million people worldwide are chronically infected by the hepatitis B virus. Despite of increased amount of previously immunized persons, significant number of children is still infected each year, often developing chronic infection and requiring appropriate follow up and treatment [1].
Literature data over wise reveals that effective and safe antiviral therapies are adopted for adults and only few labels are required for children. An accurate selection of them should improve low risk of antiviral resistance. And, of course, the clinical approach to children like active carriers of the virus and sick ones is still urgently evolving [6].
It is well known that the U.S. Food and Drug Administration approved only five medications for treatment of children with chronic hepatitis B: interferon-α, lamivudine, adefovir, entecavir and, recently, tenofovir. Some of them have certain considerations for usage depending on age limits and features of viral overload. For instance, interferon-α can be used in children older than 12 months of age, lamivudine starting at 3 years of age, adefovir and tenofovir in children aged 12 years and older, and entecavir starting from 16 years of age [1].
At the same time, the issue of asthenia development at a number of chromic somatic and infectious diseases in childhood, as well as therapy of violations of psychoemotional status, remains understudied.
Definition of asthenia has its own certain features but sometimes physicians make serious mistake, and mix it with intoxication and general weakness, knowing only general description.
Thus asthenic syndrome as a manifestation of a number of somatic, infectious and psychoneurological diseases can be often found in a pediatrician’s practice [4].
What is it asthenia in general? Asthenia (from Greek asthèneia — weakness, feebleness) — is a pathological state that declares itself by general weakness, increased fatigability, emotional lability, hyperesthesia and disorder of the basic circadian biorhythms of an organism [5]. Asthenia arises as a result of a quick exhaustion of nervous and adaptive processes, weakening or full loss of the ability to long physical and mental tension [4, 5].
It should be noted that physical and mental fatigue at asthenia does not disappear even after a long rest unlike tiredness that is a normal reaction to a serious physical or psychoemotional load [5].
Increased fatigability of a child is the most frequent complaint with which parents of the patients apply to a specialist [5]. The situation becomes more complicated by creation of an unfavourable clinic-and-paraclinic background on which other pathologic symptom complexes and diseases can be «thread» [2, 3].
Objective. To study the peculiarities of the course of the asthenic syndrome at chronic viral hepatitis in children.
Material and Research Methods
It was examined 50 school-aged children who received in-patient treatment in an Endocrine Department with gastroenterological beds of the OCCH in the city of Ivano-Frankivsk with the diagnosis chronic hepatitis verified in accordance with the Order of the MHP of Ukraine № 438 of May 26, 2010 «On introduction of a children treatment protocol majoring in «Pediatric Gastroenterology». The level of average molecules was calculated with the help of a screening method in modification of N.I. Gabrielian [1]. In addition to this, it was performed a determination of heart rate variability (HRV) for all children (apparatus CardioLab HRV, Kharkiv). When performing the analysis of HRV only «short» records of cardiac activity with the duration up to a few minutes were taken into consideration. The following spectral indices of a heart rate were calculated: total power (ТР) — total power of a spectrum in the frequency range up to 0.4 Hz that characterizes the limit of general heart rate variability; SDNN, mc — summary index of PR intervals range variability for a certain period of time that characterizes a general state of vegetative nervous system regulating mechanisms; rMSSD, mc — a square root of the sum of squares of difference of quantities of successive pairs of normal intervals NN; pNN50, mc-percent NN50 from the general number of successive pairs of intervals that differ one from another more than for 50 milliseconds; low frequency (LF) — spectrum power on the frequency 0.05–0.15 Hz; HF (high frequency) — spectrum power on the frequency 0.15–0.4 Hz. LF/HF — ratio of low- and high-frequency components, index of balance of sympathetic and parasympathetic parts of autonomic nervous system.
Results of Examination and Their Discussion
In 70.0 % of children there was confirmed the diagnosis of viral hepatitis B, in 28.0 % of patients — hepatitis С respectively. Mixed hepatitis (В + С) was found in 2.0 % of patients who were under our observation. The age of the most of the examined people (80.0 %) with viral hepatitis B was 13.0 ± 1.5 years, and the children with hepatitis С (90.0 %) — 16.0 ± 2.0 years.
Experience of both diseases to the moment of admission to hospital was 5.0 ± 2.5 years (75.0 %), in addition to that primary chronic forms were found in the half of the examined with viral hepatitis C and only in one third of children with viral hepatitis B. In the anamnesis of patients with hepatitis B the following were marked as causes of the disease development: drugs infusion (70.0 %), blood transfusion (25.0 %), surgical intervention (5.0 %). In most patients with hepatitis C the main cause of the disease remained uncertain, and in 15.0 % of patients there were observed iatrogenic factors, in particular introduction of blood preparations, harmful effects of medicine. And only 2.0 % of patients, mostly of early adulthood, observed infection in the result of insecure sexual act.
In the clinical picture of both diseases prevailed an obliterated, low-expressive symptomatology.
Yes, at hepatitis B in children to the fore came symptoms of asthenia as well as dyspeptic phenomena: decrease, more rarely — distortion of an appetite (80.0 %), bitter eructation (75.0 %), nausea (68.0 %), feeling of heaviness and spreading in epigastric area, emptying instability (50.0 %). Jaundice was not found in any child that was under our observation, only a sub-icteritiousness in one boy with mixed hepatitis.
Pain abdominal syndrome was also ill-defined in both groups of patients and had non-specific character.
Yes, in 50.0 % of the examined people with chronic viral hepatitis B there appeared a constricting pain after mistakes in a diet, in particular because of fried food and a glass of beer.
A hepatomegaly up to 1.5–2 cm (more rarely — a splenomegaly) was detected in the majority of the examined people with the help of palpation.
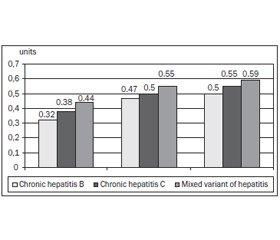
It is known that the level of average molecules serves as one of integral criteria of chronic intoxication in children with chronic hepatitis (Fig. 1).
/26/26.jpg)
As it can be seen from the provided data, the level of average molecules was reliably higher in children with chronic hepatitis C and mixed hepatitis which indicates more severe course of these diseases.
We diagnosed certain differences of heart rate variability at chronic hepatitis B and C in children (Table 1).
Time-line and spectroscopic analysis of heart rate variability provided in the Table 1 showed the decrease of the LF index as compared to eutonia (p < 0.05) that confirms the shift of vegetative balance to the side of parasympathotonia. Total power of the spectrum was lower than standard values that indicated the weakening of sympathetic influences on myocardium.
By determination of the index of regulatory systems activity, the following spectrum of pathological states was established at chronic hepatitis B in children: in 60.0 % — full-blown functional tension of index of activity of the regulatory systems (IARS = 5.6), in 25.0 % — full-blown functional tension (IARS = 7.8) relatively. Moderate functional tension of adaptation systems was detected in 20.0 % of patients with chronic hepatitis B. Hepatitis C was distinguished by deadaptation prevalence — in 80.0 % of children there could be found a full-blown functional tension of index of activity of the regulatory systems (IARS = 5.6) while moderate functional tension could be found only in 5.0 % of the examined people. At mixed hepatitis there was marked only destabilization of the given index.
In general, it should be mentioned that symptoms of asthenia arose as a rule on the base of changed constitutional background: the major part of the patients (80.0 %) suffered from nervous break-down, enuresis, stammer or nervous tic.
Characteristic of the asthenic syndrome in children with viral hepatitides is represented in Fig. 2.
/27/27_2.jpg)
As it can be seen form the presented data, psychasthenia and somatogenic asthenia prevailed in children with viral hepatitides. The encephalasthenia could be found comparatively more rarely. It is known that psychasthenia is a reaction of exhausted state of mind to a psycho-traumatic situation or a stress (in the given case the fact of a diseases itself). As a rule, this category of patients included children of asthenic body-build from families of neurasthenics the relatives of which are emotionally labile and «come into a disease» fast. Children of this group of patients more often complained about unsatisfactory conditions of stay in an in-patient department (45.0 %), ineffectiveness of provided treatment (30.0 %), fear of manipulations (25.0 %).
In the state of fatigue there occurred the affective splashes due to different inessential causes, appeared irritation and suspicion that were quickly changed by tears.
In the majority (90.0 %) of cases of somatogenic asthenia provoked by the disease itself there could be observed bad attention focusing, restlessness, increased fatigability, tearfulness and work decrement. Unmotivated mood swings and its frequent changes were observed in one third of the examined people among which dominated patients with chronic hepatitis C.
The main complaints of children with cerebrasthenia were: headache and dizziness (60.0 %), forgetfulness and non-concentration (20.0 %), inattention (10.0 %), vestibular disorders (5.0 %). It is difficult for them to study because of bad memorability of material and concentration of attention. Low self-appraisal, doubts and worries on the background of a severe disease make such children unsociable, irresolute, the one who do not believe in their own recovery or a full life with a disease.
Conclusions
1. Chronic viral hepatitis remains an actual problem of pediatric gastroenterology and, regardless of a clinical form, is accompanied by evident symptoms of asthenia and deadaptation.
2. Chronic hepatitis С, as well as mixed forms (hepatitis В + С), are characterized by the dominance of somatogenic asthenia, more rarely psychasthenia, manifestations of deadaptation (evident tension of regulatory systems index, prevalence of sympathicotonia) as well as a high level of endogenous intoxication.
Perspectives of further researches. To observe the effectiveness of therapy of viral hepatitides in catamnesis.
1. Paganelli M., Stephenne X., Sokal E.M. Chronic hepatitis B in children and adolescents / M. Paganelli, X. Stephenne, E.M. Sokal // J. Hepatol. — 2012. — 57. — P. 885-896.
2. Gabrielian N.I. Endogenous intoxication / N.I. Gabrielian //Thesis of reports of the I All-Soviet Convention of Toxicologists. — Rostov-on-Don, 1986. — P. 416-417.
3. Goracheva L.G. Diagnostics and treatment of viral hepatitides B and C in children of infants / L.G. Goracheva, I.V. Shylova // Doctor. — 2006. — № 8. — P. 32-35.
4. Zaitsev I.А. Viral hepatitis В in questions and answers / I.A. Zaitsev, А.А. Zaplatnaya. — K., 2006. — 112 p.
5. Kramarev S.А. Modern possibilities of treatment of chronic viral hepatitides in children / S.А. Kramarev, I.V. Shpak, L.А. Bolshakova // Clinic Pediatrics. — 2007. — № 4(7). — P. 120-122.
6. Lok A.S. Chronic hepatitis B: update 2009 / A.S. Lok, B.J. McMahon // Hepatology. — 2009. — 50. — P. 661-662.
7. Lytvyn L. Asthenic syndrome in children / L. Lytvyn // Baby health. — 2012. — № 5 (32). — P. 7-11.

/27/27.jpg)